Bladder Spasms
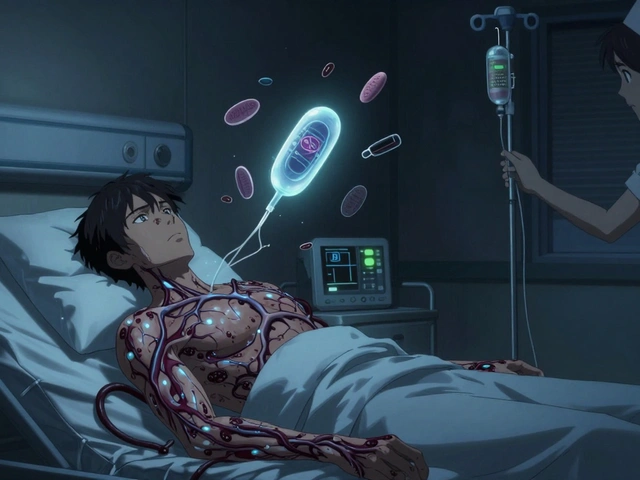
When dealing with bladder spasms, bladder spasms, involuntary contractions of the urinary bladder that cause sudden urgency, leaking, or pain. Also known as urinary bladder cramps, they are a hallmark of several urinary disorders. Overactive bladder is the most common condition that includes these spasms, while anticholinergic medication and detrusor muscle play key roles in the mechanism and treatment.
Semantic Triple: Bladder spasms are involuntary detrusor muscle contractions. Bladder spasms can be triggered by nerve irritation. Effective relief requires a combination of medication, bladder training, and lifestyle adjustments. Understanding how these entities interact helps you choose the right relief strategy and avoid unnecessary frustration.
What Triggers the Spasms?
The detrusor muscle, which lines the wall of the bladder, is controlled by a delicate balance of nerves and chemicals. When this balance tips—due to infection, caffeine, alcohol, stress, or pelvic floor weakness—the muscle can fire off sudden, unwanted contractions. Many patients discover that a hidden urinary tract infection (UTI) fuels their symptoms, while others notice that long periods of bladder holding increase the frequency of spasms. In some cases, chronic conditions like interstitial cystitis or neurological disorders such as multiple sclerosis disrupt signaling pathways, leading to persistent urgency. Recognizing the root cause is essential because treatment varies: a short course of antibiotics clears an infection, whereas lifestyle tweaks like limiting bladder irritants and practicing timed voiding help manage nerve‑driven spasms. Research shows that pelvic floor physical therapy strengthens supporting muscles, reducing the intensity of detrusor overactivity and giving patients more control.
When it comes to medication, anticholinergic drugs—such as oxybutynin and tolterodine—work by blocking the receptors that tell the detrusor muscle to contract. For patients who can’t tolerate anticholinergics, beta‑3 agonists like mirabegron relax the bladder muscle through a different pathway, offering an alternative route to relief. In more severe cases, physicians may recommend Botox injections directly into the detrusor muscle; the toxin temporarily paralyzes overactive fibers, extending the interval between bathroom trips. Alongside drugs, bladder training programs teach you to gradually increase the time between voids, retraining the nervous system to tolerate fuller bladders. Simple habits—staying hydrated, avoiding bladder irritants, and practicing proper posture when using the restroom—can make a noticeable difference.
Below you’ll find a curated collection of articles that dig deeper into each of these topics. Whether you’re looking for the latest on anticholinergic options, tips for bladder‑friendly nutrition, or step‑by‑step guides for pelvic floor exercises, the posts provide actionable insights you can start using today. Browse the list to discover practical solutions that match your situation and help you regain control over unwanted bladder spasms.
Learn how to stay active despite bladder spasms with safe exercise ideas, hydration tips, pelvic floor training, and when to seek medical help.