Bladder Spasms & Exercise Planner
Quick Takeaways
- Understand what triggers bladder spasms before you start moving.
- Low‑impact cardio and gentle strength work are usually safest.
- Stay hydrated, limit caffeine, and schedule bathroom breaks around workouts.
- Pelvic floor training can reduce spasm frequency.
- Seek medical advice if spasms persist despite lifestyle changes.
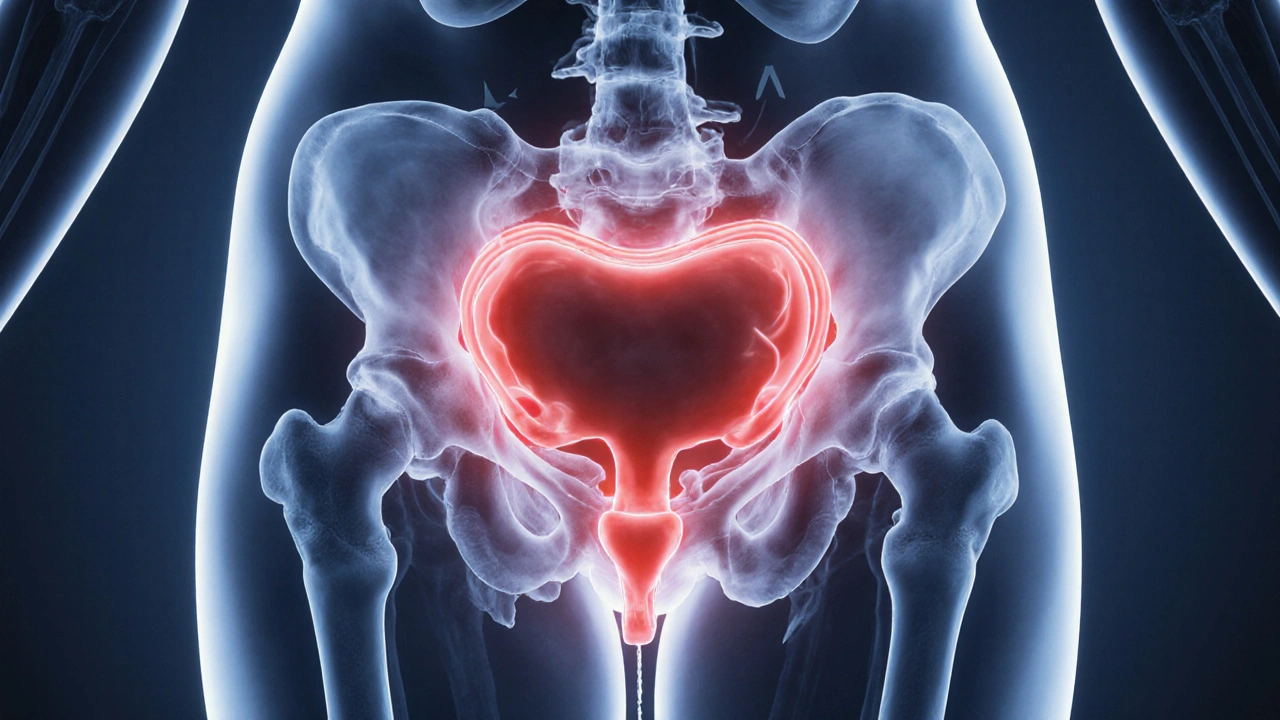
What Are Bladder Spasms?
When the Bladder spasms are involuntary contractions of the detrusor muscle that cause sudden urges to urinate, they can interrupt daily life and make exercise feel risky. The detrusor muscle, part of the urinary bladder wall, normally contracts to empty the bladder. In some people, it contracts unexpectedly, creating a sharp pressure sensation and sometimes leakage.
These episodes are often linked to a condition called overactive bladder a syndrome marked by frequent urges, nighttime urination, and occasional incontinence. While overactive bladder is a medical diagnosis, bladder spasms can also appear without a formal condition, triggered by stress, certain foods, or dehydration.
How Exercise Interacts With the Bladder
Physical activity influences bladder function in several ways. High‑impact moves-like jumping or heavy lifting-jolt the pelvis, squeezing the bladder and potentially provoking a spasm. On the flip side, regular movement improves circulation to pelvic organs, helping the detrusor muscle relax over time.
Key factors that determine whether a workout helps or harms include:
- Intensity: Sudden spikes in heart rate raise abdominal pressure.
- Duration: Long sessions without bathroom breaks can fill the bladder.
- Type of movement: Some activities compress the pelvic floor more than others.
Understanding these mechanisms lets you choose exercises that keep you moving without setting off a spasm.

Core Strategies for Safe Exercise
Below are practical steps you can adopt right away.
- Plan bathroom breaks: Schedule a restroom stop 15minutes before you begin and another midway through longer workouts.
- Stay well‑hydrated, but avoid gulping large volumes right before exercising. A steady sip of water every 15minutes works best. Hydration maintains bladder capacity and reduces irritation helps the detrusor muscle stay calm.
- Limit bladder irritants such as caffeine, alcohol, and carbonated drinks. Caffeine, for example, can increase detrusor activity and raise spasm frequency. Caffeine a known bladder stimulant that can trigger urgency is best kept to a minimum on training days.
- Choose low‑impact cardio like brisk walking, swimming, or stationary cycling. These aerobic exercise activities that raise heart rate without heavy pelvic compression keep blood flowing without jolting the bladder.
- Integrate gentle strength work. Focus on upper‑body and core moves that avoid excessive Valsalva breathing (holding breath while lifting). When you do lower‑body work, use lighter loads and higher repetitions.
- Activate the pelvic floor before, during, and after exercise. Simple Kegel contractions-tightening the muscles you’d use to stop urine flow-train the pelvic floor muscles a group of muscles that support the bladder and urethra to respond better to pressure changes.
- Consider biofeedback or physical therapy if spasms persist. Biofeedback a technique that uses sensors to teach control over pelvic muscles can be combined with tailored exercise plans for lasting relief.
Sample Workout Plan
This routine blends cardio, strength, and pelvic‑floor training. Adjust timing based on your personal bladder schedule.
| Exercise | Risk Level | Benefits | Tips for Spasm Management |
|---|---|---|---|
| Brisk Walking (30min) | Low | Improves circulation; gentle on pelvis | Take a bathroom break before starting; wear supportive shoes. |
| Swimming (20min) | Low‑Medium | Full‑body workout; water pressure can soothe pelvic muscles | Use the pool restroom beforehand; avoid chlorine‑heavy pools if they irritate skin. |
| Cycling (stationary, 20min) | Medium | Boosts leg strength; low impact on joints | Keep seat height high to reduce perineal pressure; pause every 5min for a quick Kegel. |
| Upper‑body circuit (3sets) | Low | Builds functional strength | Exhale on effort; avoid breath‑holding. |
| Body‑weight squats (2sets of 15) | Medium | Engages core & lower body | Use shallow depth; focus on steady breathing. |
| Kegel series (5×10sec hold) | None | Strengthens pelvic floor | Do after each cardio segment to reset muscle tone. |
When to Seek Professional Help
If you notice any of the following, book an appointment with a urologist or physiotherapist:
- Spasms occurring more than three times a day despite lifestyle changes.
- Visible leakage during or after exercise.
- Painful urgency or burning sensation.
- Sudden change in urinary patterns after starting a new workout routine.
Medical options may include anticholinergic medications, neuromodulation therapy, or targeted pelvic‑floor rehabilitation. Combining these with the exercise tips above often yields the best results.

Common Myths About Exercise and Bladder Health
Myth 1: You must stop all sports if you have bladder spasms.
Fact: Most activities can be modified to stay safe. The key is smart planning, not quitting.
Myth 2: Drinking a lot of water before a workout will prevent spasms.
Fact: Over‑filling the bladder raises pressure and can trigger a spasm. Aim for steady hydration instead of large pre‑workout gulps.
Myth 3: Only older adults experience bladder issues.
Fact: Young athletes, especially those with high‑intensity training schedules, also report spasms. Age isn’t the only factor.
Putting It All Together
Staying active while managing bladder spasms is a balance of timing, choice of exercise, and attention to lifestyle triggers. By planning bathroom breaks, staying hydrated without overloading, limiting caffeine, and incorporating pelvic‑floor work, most people can keep moving without constant interruptions.
Remember, your body will give you signals. If spasms persist despite these adjustments, don’t hesitate to get a professional evaluation. The right combination of medical care and tailored activity can let you enjoy both health and fitness.
Frequently Asked Questions
Can yoga help reduce bladder spasms?
Yes. Gentle yoga poses that stretch the pelvic floor, like child's pose and supine twists, can promote relaxation of the detrusor muscle. Pairing yoga with focused breathing reduces abdominal pressure and may lower spasm frequency.
Is it safe to run if I get bladder spasms?
Running can be safe if you keep the intensity moderate, wear supportive footwear, and schedule a bathroom break before hitting the pavement. If you notice spasms during high‑intensity sprints, switch to a lower‑impact cardio option like cycling.
How much water should I drink on workout days?
Aim for about 500ml (17oz) spread evenly before, during, and after exercise. Adjust based on sweat rate, temperature, and personal comfort-avoid drinking a large cup right before starting.
Do pelvic floor exercises replace other treatments?
They complement, not replace, medical options. For mild cases, consistent Kegel work may be enough. More severe spasms often need medication or physical therapy in addition to the exercises.
Can I drink coffee if I exercise regularly?
Limit coffee to a single small cup a few hours before a workout. If you notice increased urgency after caffeine, consider switching to decaf or herbal tea on training days.









Nick Ham
6 Oct 2025 at 18:21Utilize low‑impact cardio to mitigate intra‑abdominal pressure and preserve detrusor stability.