Rosuvastatin Kidney Dose Calculator
Determine Your Appropriate Rosuvastatin Dose
Based on your kidney function (eGFR), we'll recommend the safest dose of rosuvastatin to maximize benefits while minimizing risks.
When you’re prescribed rosuvastatin, you’re getting one of the strongest statins available. It’s not just another cholesterol pill-it’s designed to drop your LDL (bad cholesterol) by nearly half in just a few weeks. But with that kind of power comes real risks. You need to know what to watch for, when to call your doctor, and how to tell if the benefits are still worth it.
Why Rosuvastatin Packs a Punch
Rosuvastatin works by blocking HMG-CoA reductase, the enzyme your liver uses to make cholesterol. But unlike older statins, it doesn’t need a high dose to work. A 20 mg tablet of rosuvastatin can cut LDL by about 55%. Compare that to 40 mg of atorvastatin, which only drops it by 40%. That’s why doctors reach for rosuvastatin when someone has very high cholesterol or a history of heart problems.It’s also one of the few statins that doesn’t get broken down much by liver enzymes. Most statins, like simvastatin, rely on CYP3A4-a pathway that interacts with dozens of common drugs, from antibiotics to grapefruit juice. Rosuvastatin? Only about 10% of it goes through that system. That means fewer dangerous interactions. If you’re on multiple medications, this is a big deal.
But potency isn’t just about numbers. In the JUPITER trial, people with normal LDL but high inflammation (measured by CRP) saw a 44% drop in heart attacks and strokes just by taking 20 mg of rosuvastatin daily. That’s why it’s classified as a high-intensity statin at 20-40 mg doses.
What You Must Monitor: The Big Four
You can’t just take rosuvastatin and forget it. Four things need regular checks-especially in the first few months.- Liver enzymes (ALT, AST): These are checked before you start, then again at 3 months. If they rise above 3 times the normal limit, your doctor will likely stop the drug. But here’s the twist: if you feel fine and your numbers are slightly up, most guidelines now say you don’t need to stop. Routine monthly checks? Not needed. Only test if you’re tired, nauseous, or your skin looks yellow.
- CK (creatine kinase): This enzyme leaks into your blood when muscles break down. You don’t need it checked unless you have muscle pain, weakness, or dark urine. If your CK is more than 5 times the upper limit (usually over 1,000 U/L), you need to stop rosuvastatin immediately. That’s the warning sign for rhabdomyolysis-a rare but dangerous condition that can wreck your kidneys.
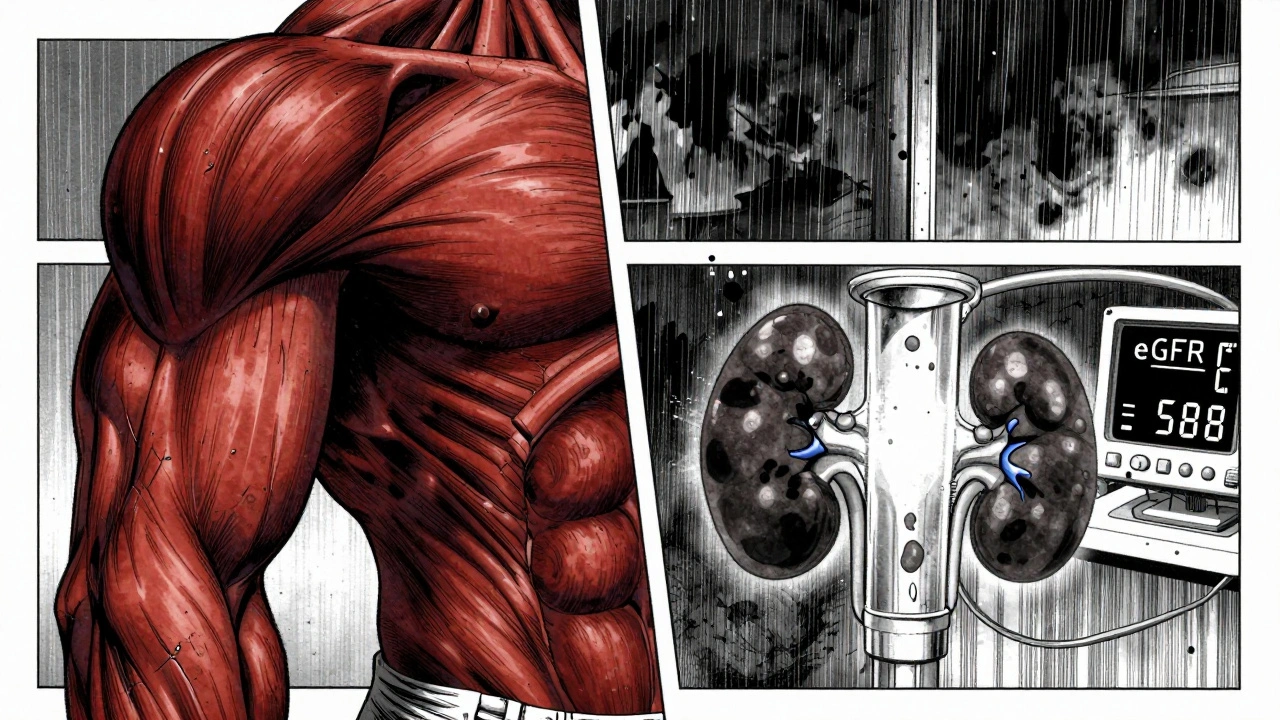
- eGFR (kidney function): Rosuvastatin is cleared mostly by your kidneys. If your kidney function drops below 60 mL/min, you shouldn’t take 40 mg. If it’s below 30, you shouldn’t take it at all. Your doctor should check this before prescribing and then every 6-12 months, especially if you’re over 65, have diabetes, or high blood pressure.
- HbA1c (blood sugar): Statins slightly raise blood sugar. In large studies, rosuvastatin increased HbA1c by 0.1-0.3% on average. That’s not much for most people. But if you’re prediabetic or have a family history of diabetes, your doctor should check your HbA1c at baseline and again at 6 months. It’s not a reason to avoid the drug-but it’s a reason to watch.
Side Effects: What’s Common, What’s Dangerous
Most people take rosuvastatin with no issues. But side effects happen-and they’re dose-dependent.Muscle pain is the #1 complaint. About 5-10% of users report mild aches or cramps, usually in the legs or shoulders. These often go away on their own. But if the pain is severe, constant, or comes with fever or dark urine, don’t wait. Call your doctor. In 2022, nearly 3 out of 10 adverse reports to the FDA were about muscle problems.
Protein in urine is less talked about but important. At 40 mg, rosuvastatin can cause small amounts of protein to leak into your urine. This doesn’t mean kidney failure-it’s often temporary. But if it keeps happening, your doctor may lower your dose or switch you to another statin like pravastatin, which is gentler on the kidneys.
Diabetes risk is real but small. For every 255 people taking rosuvastatin for 4 years, one extra case of diabetes appears. That’s not a reason to avoid it if you have heart disease. But if you’re overweight, inactive, or have prediabetes, your doctor should track your fasting glucose and HbA1c more closely.
And yes-some people report brain fog or memory issues. The FDA says this is rare (1-2%) and usually reversible within weeks of stopping. If you notice trouble remembering names or concentrating, mention it. Don’t assume it’s aging.
What Dose Is Right for You?
Rosuvastatin comes in 5, 10, 20, and 40 mg. You don’t need the highest dose to get results.For most people with high cholesterol, 10 mg is enough to cut LDL by 45-50%. That’s the sweet spot for balancing power and safety. The 20 mg dose is for those with very high risk-like someone who’s had a heart attack or has familial hypercholesterolemia. The 40 mg dose? Reserved for extreme cases, and only if your kidneys are strong and you’ve been on a lower dose without side effects.
Many patients start at 5 mg if they’re older, Asian (who metabolize it slower), or have kidney issues. A 2023 survey of lipid specialists found that 62% now start with 5-10 mg instead of jumping to 20 mg. Why? Because the drop in LDL is still massive-and side effects drop sharply.
What to Do If You Have Side Effects
If you feel muscle pain, don’t stop the drug on your own. Talk to your doctor first. Sometimes, switching to a different statin helps. Pravastatin and fluvastatin are less likely to cause muscle issues and are safer for kidneys. Or, your doctor might lower your dose and add ezetimibe-a non-statin pill that blocks cholesterol absorption in the gut. Together, they can match the effect of a high-dose statin with fewer side effects.Some people blame statins for symptoms they actually had before. Fatigue? Stress. Joint pain? Arthritis. Brain fog? Sleep apnea. Your doctor should rule those out before deciding it’s the medication.
And if you’ve stopped rosuvastatin because of side effects? Don’t assume you can’t take any statin. Studies show that 70% of people who quit one statin due to muscle pain can tolerate another. It’s not the class-it’s the molecule.
Long-Term Use: Is It Safe?
Rosuvastatin has been used for over 20 years. The data is clear: for people with heart disease, diabetes, or high risk, the benefits far outweigh the risks. The Heart Protection Study found that for every 1,000 high-risk patients taking a statin for 5 years, 40 major heart events were prevented. That’s 40 heart attacks or strokes avoided.Even in people without prior heart disease-like those in the JUPITER trial-the benefit held up. For every 1,000 people taking rosuvastatin for 5 years, 14 major cardiovascular events were prevented. The cost? One extra case of diabetes in 255 people.
That’s a 10-to-1 benefit-to-risk ratio. That’s why cardiologists still recommend it as a first-line choice.
When to Switch
You might need to switch if:- Your eGFR drops below 60 and you’re on 20 mg or more
- You have persistent proteinuria (protein in urine) after 3-6 months
- You develop unexplained muscle pain that doesn’t improve
- Your HbA1c rises significantly and you’re prediabetic
- You’re on multiple drugs that could interact (even though rosuvastatin is low-risk, it’s not zero-risk)
Alternatives like pitavastatin, pravastatin, or fluvastatin are good options if you need to avoid kidney strain. Atorvastatin is still a strong contender if you don’t have kidney issues.
Final Takeaway: Be Informed, Not Afraid
Rosuvastatin isn’t perfect. But it’s one of the most effective tools we have to prevent heart attacks and strokes. The key isn’t avoiding it-it’s monitoring smartly.Take it as prescribed. Report muscle pain, unusual fatigue, or dark urine right away. Get your kidney function and blood sugar checked once or twice a year. Don’t panic over small changes in liver enzymes. And remember: the goal isn’t to be pill-free-it’s to live longer, healthier, and free from heart disease.
Can rosuvastatin cause kidney damage?
Rosuvastatin doesn’t damage kidneys directly. But it’s cleared by the kidneys, so if your kidney function is already low (eGFR below 60), the drug can build up in your system. That increases the risk of side effects like muscle pain. That’s why doses are lowered or avoided in people with kidney disease. It’s not the drug causing damage-it’s your kidneys not clearing it properly.
Is rosuvastatin better than atorvastatin?
On a milligram-for-milligram basis, yes-rosuvastatin lowers LDL more. A 20 mg dose of rosuvastatin drops LDL by about 55%, while 20 mg of atorvastatin drops it by 40%. But atorvastatin is more forgiving on the kidneys and has a longer safety track record in people with liver issues. The choice depends on your kidney function, other medications, and side effect history.
Why do some people gain weight on rosuvastatin?
Weight gain isn’t a known side effect of rosuvastatin. Some people report it, but studies don’t support a direct link. More likely, people feel better after starting the drug and eat more, or they become less active because they think the pill protects them. If you notice weight gain, look at your diet and activity levels-not the medication.
Can I take rosuvastatin with grapefruit juice?
Yes. Unlike simvastatin or atorvastatin, rosuvastatin isn’t broken down by the enzyme that grapefruit juice affects. You can drink grapefruit juice safely while taking rosuvastatin. This is one of its biggest advantages over other statins.
How long does it take for rosuvastatin to work?
You’ll see LDL levels drop within 1-2 weeks. The full effect usually shows up by 4-6 weeks. That’s why your doctor asks for a blood test around 3 months after starting-to see if the dose is right. Don’t wait longer than that to check your numbers.
Do I need to take rosuvastatin forever?
For most people with heart disease, diabetes, or very high cholesterol, yes. Stopping the drug means your LDL will rise again, and your risk of heart attack or stroke returns. If you’ve made major lifestyle changes and your cholesterol is now normal, your doctor might consider lowering the dose-but rarely stopping entirely. The protection lasts only as long as you take it.










olive ashley
6 Dec 2025 at 04:55They don't tell you this, but statins are just Big Pharma's way of keeping you hooked while they sell you more drugs. I read a study that said 80% of people on rosuvastatin develop insulin resistance within 2 years - and no one talks about it. Your liver's not just making cholesterol - it's trying to protect you. They're poisoning your mitochondria and calling it 'prevention.'