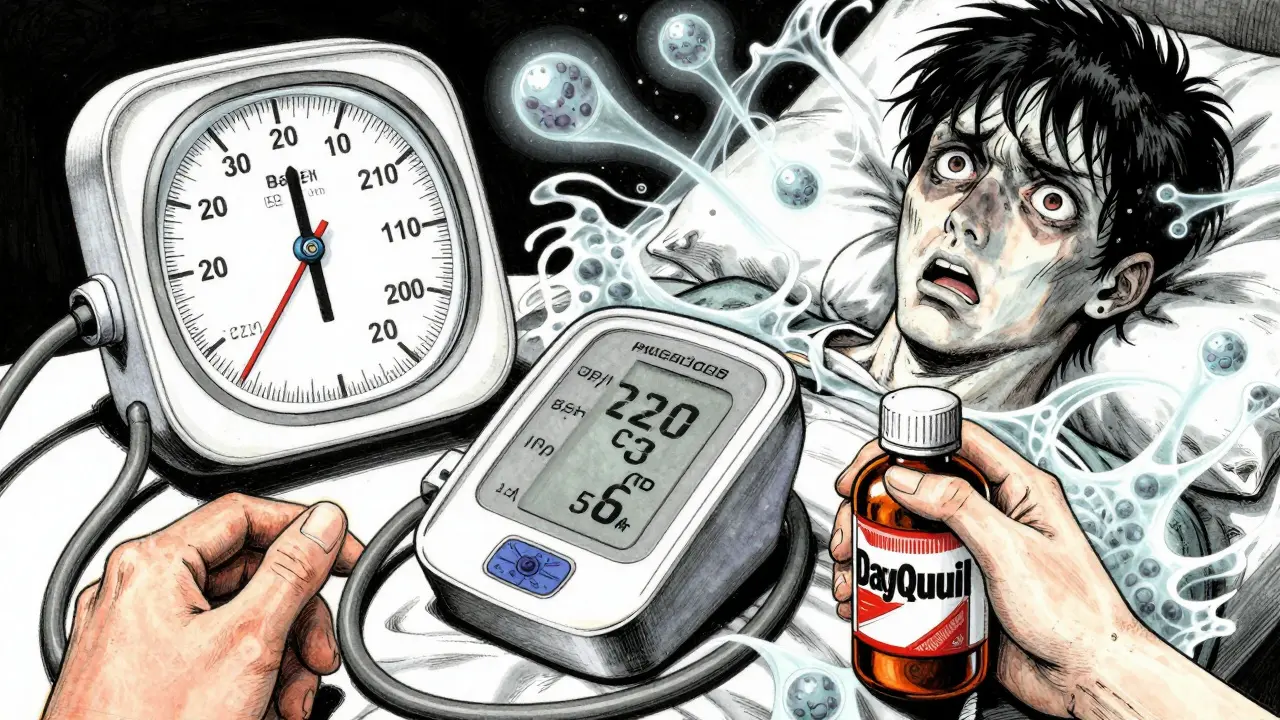
If you’re taking an MAOI for depression, a simple cold medicine could send you to the emergency room. This isn’t a hypothetical risk. It’s a real, documented danger that has landed people in hospitals with blood pressure over 220/110 - and some have nearly died from it. The problem? Many over-the-counter cold and flu products contain ingredients that interact dangerously with monoamine oxidase inhibitors (MAOIs). These aren’t rare drugs. Around 350,000 Americans still take them, mostly because other antidepressants didn’t work. But if you’re one of them, you need to know exactly what’s safe and what’s not.
What Are MAOIs and Why Do They Matter?
MAOIs - like phenelzine (Nardil), tranylcypromine (Parnate), and isocarboxazid (Marplan) - work by blocking an enzyme called monoamine oxidase. This enzyme normally breaks down neurotransmitters like serotonin, norepinephrine, and dopamine. When it’s blocked, those chemicals build up in the brain, which can lift mood in people who haven’t responded to other treatments. That’s why MAOIs are still used, even though they’re older and come with serious risks. They’re not first-line anymore, but for treatment-resistant depression, they can be the only thing that works. Success rates can hit over 50% in these cases, compared to 30-40% for SSRIs.
There’s also the transdermal patch, selegiline (Emsam). It delivers the drug through the skin, which lowers the risk of dietary interactions - but not the risk from cold medicines. Even at the lowest dose (6 mg/24hr), Emsam still carries the same danger from OTC decongestants and cough suppressants. Many people assume the patch is safer overall, but that’s not true when it comes to cold meds.
The Two Deadly Risks: Hypertensive Crisis and Serotonin Syndrome
There are two main dangers when MAOIs mix with common cold products: hypertensive crisis and serotonin syndrome. Both can be fatal.
Hypertensive crisis happens when you take a decongestant like pseudoephedrine (Sudafed) or phenylephrine (Sudafed PE). These drugs cause your body to release norepinephrine - a natural stimulant that raises blood pressure. Normally, your body breaks down excess norepinephrine with the monoamine oxidase enzyme. But if you’re on an MAOI, that enzyme is blocked. The norepinephrine builds up uncontrollably. Blood pressure spikes fast - sometimes within an hour. Symptoms include severe headache, blurred vision, chest pain, nausea, and a pounding heartbeat. In one documented case, a patient’s blood pressure hit 220/110 after taking Sudafed with Parnate. That’s higher than most people’s pressure during a heart attack. Emergency treatment was needed.
Serotonin syndrome is different. It occurs when you combine MAOIs with serotonergic drugs like dextromethorphan (found in Robitussin DM, Delsym, DayQuil, and many others). Both MAOIs and dextromethorphan increase serotonin levels. Together, they push serotonin way past safe limits. Symptoms include confusion, rapid heart rate, high fever, muscle rigidity, tremors, and seizures. The National Center for Biotechnology Information (NCBI) calls this combination “the most toxic” for serotonin syndrome. Unlike hypertensive crisis, which hits fast, serotonin syndrome can creep up over hours or days. But once it starts, it can spiral quickly.
Which Cold Medicines Are Dangerous?
Not all cold medicines are risky. But the dangerous ones are everywhere - often hidden in multi-symptom formulas. Here’s what to avoid:
- Pseudoephedrine - Sudafed, Claritin-D, Zyrtec-D
- Phenylephrine - Sudafed PE, Benadryl Allergy & Sinus, Mucinex D
- Dextromethorphan - Robitussin DM, Delsym, DayQuil, NyQuil, Theraflu
- Phenylpropanolamine - Older products, mostly banned now, but still in some foreign or vintage formulations
Here’s the kicker: 78% of OTC cold and flu products contain at least one of these ingredients, according to US Pharmacist (2023). That means if you grab a bottle off the shelf without checking, you’re more likely than not to pick something dangerous. Even “natural” or “herbal” cold remedies can contain stimulants like ephedra or yohimbine - which are also off-limits.
What Can You Safely Take Instead?
You don’t have to suffer through a cold untreated. There are safe options - you just have to be picky.
- For cough: Guaifenesin (Mucinex) - it loosens mucus and doesn’t affect neurotransmitters.
- For fever or pain: Acetaminophen (Tylenol) - it’s safe and effective. Avoid NSAIDs like ibuprofen or aspirin unless your doctor says it’s okay.
- For runny nose or sneezing: Antihistamines like loratadine (Claritin) or cetirizine (Zyrtec) - without decongestants. Stick to the plain versions.
- For sore throat: Saltwater gargles, throat lozenges without menthol or phenol (check labels), or plain honey.
Always read the “Active Ingredients” section on the label - not the brand name or marketing claims. If you see any of the risky ingredients listed, put it back. Even if the bottle says “for cold and flu,” it might still contain dextromethorphan or phenylephrine.
Why This Isn’t Just a ‘Be Careful’ Warning
This isn’t a case of “maybe don’t do this.” This is a medical emergency waiting to happen. The FDA’s Adverse Event Reporting System recorded 127 cases of hypertensive crisis linked to MAOIs and OTC cold meds between 2018 and 2022. Eighteen of those required hospitalization. One Reddit user shared how they ended up in the ER after taking Sudafed with Parnate - unaware of the risk. Another reported 12 hours of severe headache and palpitations after taking DayQuil with Nardil. Both were lucky to survive.
And it’s not just about big doses. A 2023 study from the University of Texas Southwestern showed that even a single 30mg dose of pseudoephedrine - the standard dose in one Sudafed pill - caused an average blood pressure spike of 42/28 mmHg in people on phenelzine. That’s enough to trigger a crisis in someone with even mild high blood pressure.
Doctors and pharmacists know this. The American Psychiatric Association’s 2020 guidelines say patients on MAOIs must be counseled repeatedly about these risks. But many patients don’t get that counseling. Or they forget. That’s why wallet cards - like the one one patient used for five years - are so valuable. Write down every unsafe ingredient and keep the card in your wallet or phone. Show it to pharmacists every time you buy something.
What About Switching Medications?
If you’re thinking about switching from an MAOI to something safer - like an SSRI or SNRI - don’t do it without medical supervision. You can’t just stop one and start another. Because MAOIs are mostly irreversible inhibitors, you need a 14-day washout period before starting any other antidepressant. Otherwise, you risk serotonin syndrome. The same rule applies if you’re switching to an MAOI from another drug. Your doctor will guide you through this, but it takes time and planning.
And while newer antidepressants like bupropion (Wellbutrin) have far fewer interactions, they’re not always effective for treatment-resistant depression. That’s why MAOIs still have a place - even if they’re used by less than 1% of all antidepressant users.
What’s Changing? Are Safer Options Coming?
There’s hope on the horizon. Researchers are working on reversible MAO-A inhibitors that might avoid these interactions. One compound, CX-1010, is in Phase II trials and shows promise for reducing the risk of hypertensive crisis. But it’s years away from being available.
For now, the safest option is awareness. The transdermal selegiline patch (Emsam) is becoming more popular - it now makes up 68% of all MAOI prescriptions in the U.S. But again, it doesn’t change the cold medicine risk. The patch may reduce dietary tyramine issues, but it doesn’t protect you from pseudoephedrine or dextromethorphan.
Pharmacies are slowly improving. Emsam’s patient leaflet now includes detailed lists of safe and unsafe medications - something older MAOIs didn’t have. But you can’t rely on the pharmacy to catch it. You have to be your own advocate.
Final Checklist: What to Do Today
If you take an MAOI, here’s your action plan:
- Check every medication you take - even vitamins and supplements - for pseudoephedrine, phenylephrine, or dextromethorphan.
- Keep a printed or digital list of safe alternatives (guaifenesin, acetaminophen, plain antihistamines).
- Ask your pharmacist to review every OTC purchase - even if you’ve bought it before. Formulas change.
- Carry a wallet card listing your MAOI and the dangerous ingredients to avoid.
- If you accidentally take a risky medication, monitor for symptoms: severe headache, chest pain, rapid heartbeat, confusion, fever. Go to the ER immediately if any appear.
MAOIs saved lives. But they demand respect. A cold medicine you picked up without thinking could be the one that ends it. Knowledge isn’t just helpful here - it’s the only thing standing between you and disaster.
Can I take Tylenol with MAOIs?
Yes, acetaminophen (Tylenol) is safe to take with MAOIs for pain or fever. It doesn’t interact with monoamine oxidase enzymes or affect serotonin or norepinephrine levels. Stick to the recommended dose - no more than 3,000 mg per day - and avoid combination products that include decongestants or cough suppressants.
Is Mucinex safe with MAOIs?
Only the plain version - guaifenesin - is safe. Avoid Mucinex D, Mucinex DM, or any version with “D” or “DM” on the label. Those contain pseudoephedrine or dextromethorphan, which are dangerous with MAOIs. Always read the active ingredients list, not just the brand name.
Can I use nasal sprays with MAOIs?
Topical nasal sprays like oxymetazoline (Afrin) are generally considered safer than oral decongestants because they’re absorbed in smaller amounts. But they still carry some risk, especially with prolonged use or high doses. Most experts still advise caution. If you must use one, limit it to 3 days and talk to your doctor first. Never use oral decongestants - even in spray form - if you’re on an MAOI.
What happens if I accidentally take Sudafed with an MAOI?
Monitor closely for symptoms: severe headache, blurred vision, chest pain, rapid heartbeat, nausea, or anxiety. Blood pressure can spike within minutes. If you feel any of these, go to the emergency room immediately. Do not wait. Bring your medication list with you. Emergency treatment may include medications like nitroprusside or phentolamine to rapidly lower blood pressure.
Are there any cold medicines labeled as safe for MAOI users?
No OTC cold medicine is officially labeled “safe for MAOI users.” Manufacturers don’t list that because the risk is too high and variable. Instead, rely on ingredient lists and trusted resources like the MAOI Nutrition Support website or your pharmacist. Stick to single-ingredient products with known safe components: guaifenesin, acetaminophen, or plain antihistamines like loratadine.











Peter Ronai
17 Dec 2025 at 08:17Let me be crystal clear-this isn’t just ‘cautionary advice.’ It’s a death sentence waiting for a pharmacy clerk to miss a red flag. I’ve seen two friends in ICU from this exact combo. One took DayQuil thinking ‘it’s just a cough syrup.’ He woke up screaming in the ER with a BP of 230/120. No joke. This isn’t about being paranoid-it’s about being alive.