HIT Risk Calculator
Calculate the probability of Heparin-Induced Thrombocytopenia using the standard 4Ts clinical scoring system. This tool helps estimate your risk based on key clinical factors.
Important Note
This calculator estimates clinical probability using the 4Ts scoring system. It is for educational purposes only and should not replace clinical judgment. Always consult with a healthcare provider for diagnosis and treatment decisions.
Most people think of heparin as a simple, safe way to prevent blood clots. It’s used in hospitals every day - after surgery, in intensive care, even to keep IV lines open. But for a small number of patients, this common drug triggers a dangerous paradox: instead of stopping clots, it starts them. That’s heparin-induced thrombocytopenia - or HIT. It’s rare, but when it happens, it can be life-threatening.
What Exactly Is HIT?
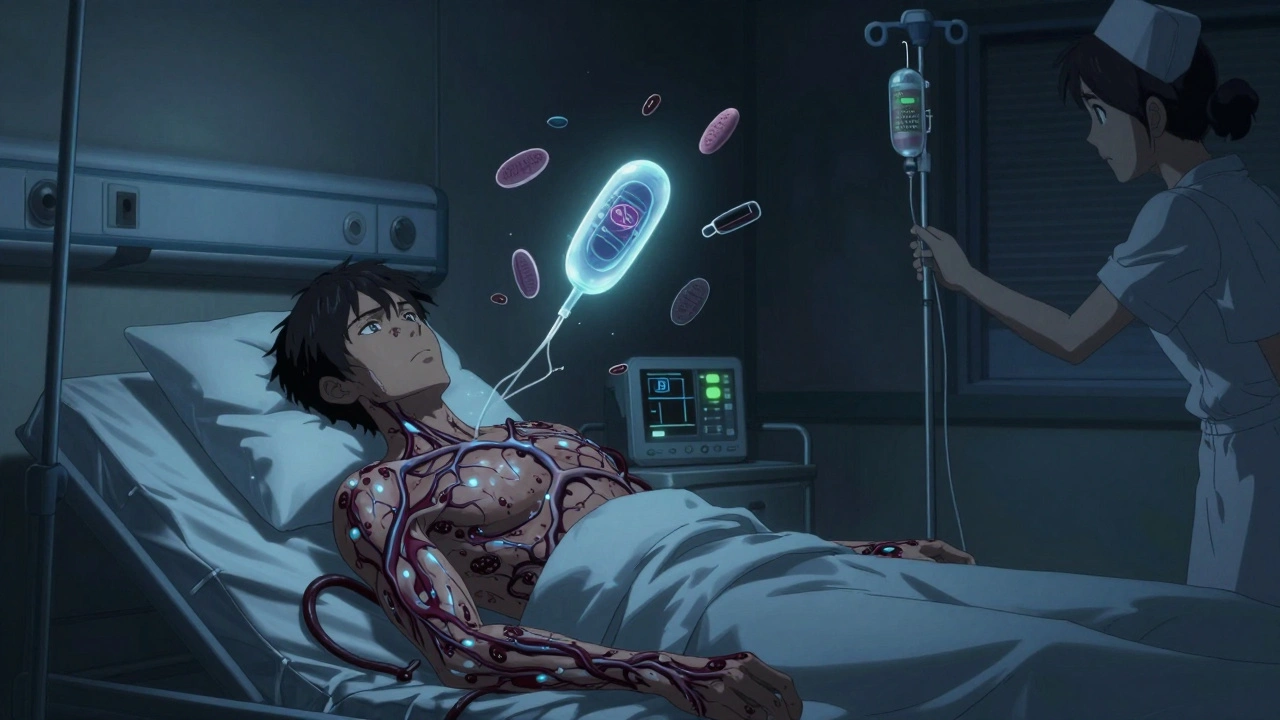
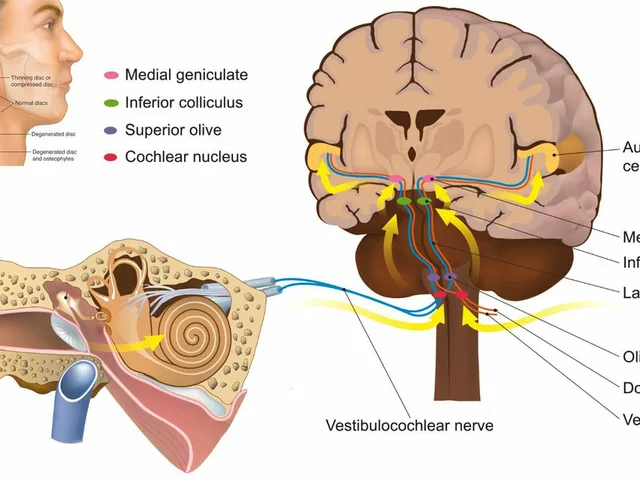
HIT isn’t just a drop in platelets. It’s an immune reaction. Your body mistakes a combination of heparin and a protein called platelet factor 4 (PF4) as something foreign. It makes antibodies against it. Those antibodies stick to your platelets and make them go crazy - clumping together, activating, and triggering clots all over your body. At the same time, those platelets get used up. So your platelet count drops. You have fewer platelets, but you’re more likely to clot. That’s the dangerous twist.There are two types of HIT. Type I is mild, happens within the first couple of days, and doesn’t need treatment. It’s not the real problem. Type II is the one doctors worry about. It shows up 5 to 14 days after starting heparin. If you’ve had heparin in the last 100 days, it can hit even faster - sometimes in just 1 to 3 days. That’s because your body already has the antibodies waiting.
Who’s at Risk?
Not everyone gets HIT. But some people are much more likely to. Women are 1.5 to 2 times more likely than men. People over 40 face a 2 to 3 times higher risk than younger patients. The biggest risk? Orthopedic surgery - especially hip or knee replacements. Up to 10% of patients after these procedures develop HIT. Cardiac surgery patients are next, with 3 to 5% risk. Medical patients on heparin for other reasons? Around 1 to 3%.The type of heparin matters too. Unfractionated heparin - the older, stronger version - carries a 3 to 5% risk. Low molecular weight heparin (like enoxaparin) is safer, but still causes HIT in 1 to 2% of cases. Even small amounts can trigger it. Heparin flushes, heparin-coated catheters, or IV lines with heparin in them? They’ve caused HIT too. About 15 to 20% of cases come from these sources.
Duration matters. If you’ve been on heparin for less than 4 days, your risk is under 0.5%. Between 5 and 10 days? Risk jumps to 3 to 5%. Beyond 10 days? It hits 5 to 10%.
What Are the Symptoms?
HIT doesn’t always scream for attention. But when it does, it’s urgent. The most common sign? A sudden drop in platelets - usually 30% to 50% below your normal level. But platelets alone don’t tell the whole story. The real danger is clots.Half of all HIT patients develop serious clots. Deep vein thrombosis (DVT) happens in 25 to 30% - that’s swelling, pain, warmth, and redness in the leg. Pulmonary embolism (PE) hits 15 to 20% - sudden shortness of breath, chest pain, fast heart rate. These aren’t rare side effects. They’re the main reason HIT kills.
Other signs include skin changes. Bruising, black spots, or blue discoloration right where the heparin was injected. Sometimes it spreads to fingers, toes, nose, or nipples. That’s called skin necrosis - and it’s a red flag. Fever, chills, dizziness, anxiety, and sweating can also show up. They’re not specific to HIT, but if they come with a low platelet count and recent heparin use, it’s time to suspect HIT.

How Is It Diagnosed?
Doctors don’t just order a blood test and assume it’s HIT. They use a tool called the 4Ts score. It looks at four things:- Thrombocytopenia - how low are your platelets?
- Timing - when did the drop happen after heparin started?
- Thrombosis - are there new clots?
- Other causes - is there something else that could explain the low platelets?
A score of 6 to 8 means high probability. 4 to 5 is intermediate. 0 to 3 is low. If your score is low, HIT is unlikely - no need for expensive tests. If it’s high, you get lab tests. First, an immunoassay - it checks for antibodies. It’s 95% sensitive, so it catches almost all real cases. But it also gives false positives. That’s why the next test is critical: the serotonin release assay. It’s the gold standard. It’s 99% specific. If it’s positive, you have HIT.
Even with the best tests, 1 in 1,000 patients gets a false negative. That’s why doctors don’t wait for test results if the clinical picture is clear. If you’re on heparin, your platelets dropped sharply, and you’re developing clots - stop heparin immediately. Don’t wait for the lab.
What Happens If You Get HIT?
The first rule? Stop all heparin - every last bit. That includes flushes, heparin-coated catheters, even heparin lock solutions. Any heparin in your system can make things worse.You need a different blood thinner - one that doesn’t trigger HIT. The options:
- Argatroban - given by IV. Used if you have liver problems. Dose is adjusted based on blood tests.
- Bivalirudin - also IV. Preferred in heart surgery patients.
- Fondaparinux - a once-daily shot. Now recommended as first-line for non-life-threatening cases. It’s effective in 92% of cases.
- Danaparoid - available in some countries. Not in the U.S.
Never start warfarin alone during HIT. It can cause skin necrosis - the same blackening you see in HIT. Only add warfarin after your platelets recover to over 150,000 and you’ve been on the alternative drug for at least 5 days.
How long do you stay on the new blood thinner? If you had HIT without clots, 1 to 3 months. If you had clots - HITT - you need 3 to 6 months. Some people need lifelong anticoagulation if they’ve had repeat events.

Why Does This Happen So Often?
Heparin is used in over 1 million patients every year in the U.S. That means 50,000 to 100,000 people are at risk for HIT. About 1 in 20 of those will develop it. And when HIT leads to clots - HITT - the death rate is 20 to 30% if untreated. Even with treatment, 5 to 10% of patients lose limbs.The cost is huge. A single HITT case adds $35,000 to $50,000 in extra hospital bills. That’s why hospitals now have protocols: check platelets every 2 to 3 days between days 4 and 14 of heparin therapy. If the count drops, trigger the 4Ts score immediately.
Doctors are getting better at spotting it. Training improves how accurately they use the 4Ts score - reliability is now 85 to 90%. But delays still happen. In 10 to 15% of cases, heparin keeps being given because doctors aren’t sure. That’s deadly.
What’s Next for HIT?
Research is moving fast. New antibody tests are being developed that focus only on PF4 - not heparin-PF4 complexes. Early results suggest they’ll cut false positives from 15% to 5%. That means fewer people get wrongly diagnosed and put on risky drugs.Scientists are also working on new anticoagulants that don’t interact with PF4 at all. Two compounds are in Phase II trials. If they work, they could replace heparin for many patients - and eliminate HIT forever.
But the big question remains: why does the immune system react this way in the first place? We still don’t fully understand what triggers the antibody formation. That’s why we can’t prevent it - only treat it after it happens.
What Patients Should Know
If you’re on heparin, watch for these signs: swelling or pain in your leg, sudden shortness of breath, unexplained bruising or dark spots near injection sites. Tell your nurse or doctor immediately. Don’t assume it’s something minor.If you’ve had HIT before, you’ll always carry the antibodies. You’ll never be able to use heparin again. Make sure your medical records clearly say "HIT: NO HEPARIN." Wear a medical alert bracelet if you can. When you go to the hospital, say it out loud: "I had HIT. I cannot have heparin."
It’s scary to think a drug meant to protect you could harm you. But awareness saves lives. Knowing the signs, asking the right questions, and demanding platelet checks can make all the difference.






Annie Grajewski
6 Dec 2025 at 04:59so like... heparin makes your platelets go 'wait wtf' and then they start clumping like a bad group project? lol. i thought drugs were supposed to fix things, not turn your blood into a horror movie. also why is this only a problem for rich people who get surgeries? why not just ban heparin already??