Starting a new medication can feel like a step toward feeling better-but it can also open the door to hidden risks. Many people don’t realize that the medicine they’re taking for high blood pressure might make their cholesterol drug less effective-or even dangerous. Drug interactions aren’t rare. In fact, drug interactions affect 3 to 5% of all outpatient prescriptions, and that number jumps to 30% if you’re taking five or more medications. If you’re over 65, you’re especially at risk: more than 40% of adults in that age group take five or more drugs regularly. The stakes are high. A single interaction can lead to hospitalization, organ damage, or worse.
What Exactly Is a Drug Interaction?
A drug interaction happens when one substance changes how another works in your body. This isn’t just about pills. It includes over-the-counter meds, supplements, herbal products, even food and alcohol. There are two main types: pharmacokinetic and pharmacodynamic.Pharmacokinetic interactions mess with how your body processes the drug-how it’s absorbed, broken down, or cleared out. The most common culprit? The CYP3A4 enzyme. It handles about half of all clinically significant interactions. For example, if you take simvastatin (a cholesterol drug) with amlodipine (a blood pressure pill), your body can’t clear the statin fast enough. That builds up toxic levels in your muscles. The fix? Keep simvastatin under 20 mg per day if you’re on amlodipine. If you’re on diltiazem or verapamil, drop it to 10 mg. That’s not a suggestion-it’s a safety limit backed by clinical data.
Pharmacodynamic interactions are about effects, not metabolism. Think of it like stacking two sedatives: opioids and promethazine. Together, they don’t just add up-they multiply. Studies show this combo can increase drowsiness and breathing problems by 200 to 300%. Same goes for blood thinners. Mixing low molecular weight heparin with a DOAC like rivaroxaban can spike your bleeding risk by 300 to 400%. No gray area here. This combo should be avoided entirely unless under strict hospital supervision.
High-Risk Combinations You Need to Know
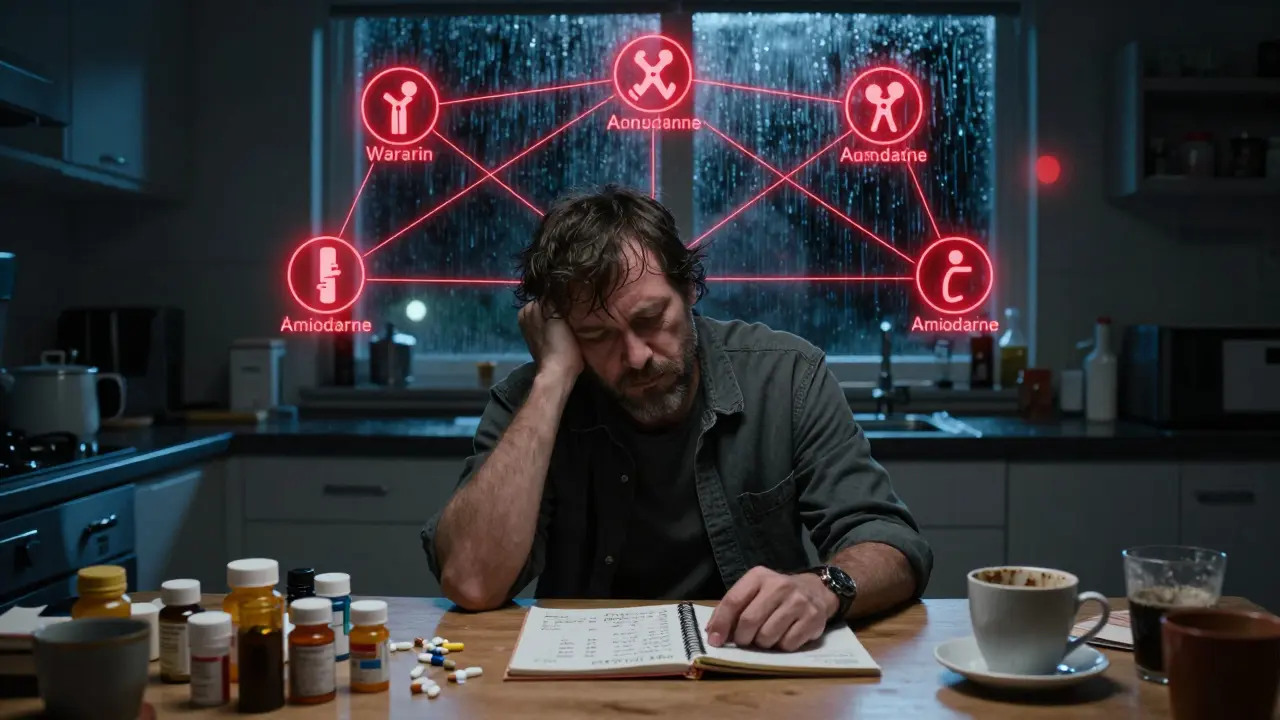
Some interactions are so dangerous they’re considered medical emergencies. Here are a few you shouldn’t ignore:- Warfarin + Amiodarone: Amiodarone (used for irregular heartbeat) slows down how warfarin breaks down. Your INR can skyrocket in days. Doctors recommend cutting warfarin by 30 to 50% right away-and checking your INR within 3 to 5 days of starting amiodarone.
- MAO Inhibitors + Tyramine-Rich Foods: Drugs like phenelzine (Nardil) can cause a deadly spike in blood pressure if you eat aged cheese, cured meats, or tap beer. One case reported systolic pressure over 200 mmHg after eating just one slice of cheddar. That’s not a myth-it’s documented.
- St. John’s Wort + Antivirals or Immunosuppressants: This popular herbal supplement can slash blood levels of cyclosporine, HIV meds, and even birth control pills by 40 to 60%. Most patients never tell their doctor they’re taking it.
- Calcium Channel Blockers + Simvastatin: As mentioned, dose limits exist for a reason. Exceeding them can cause rhabdomyolysis-a condition where muscle tissue breaks down and can destroy your kidneys.
How to Protect Yourself
You don’t need to be a doctor to avoid these risks. Here’s how to stay safe:- Make a complete list of everything you take. Not just prescriptions. Include vitamins, herbal teas, CBD oil, pain relievers, and even antacids. Write down the dose and how often you take it. Bring this list to every appointment.
- Ask your pharmacist to review it. Pharmacists catch 40 to 60% more interactions than doctors alone during medication reconciliation. They’re trained to spot these things. Don’t assume your doctor knows every supplement you’re using-many patients don’t mention them.
- Check for red flags. If you start a new drug and suddenly feel dizzy, nauseous, weak, or notice unusual bruising or swelling, don’t wait. Call your provider. These aren’t just side effects-they could be signs of a dangerous interaction.
- Know your triggers. Some drugs need an empty stomach. That means no food for 1 hour before and 2 hours after. Not “don’t eat dinner.” Not “wait two hours after your meal.” One hour before. Two hours after. Misunderstanding this is one of the most common reasons meds don’t work-or cause side effects.
The Role of Technology-and Why It Falls Short
Most clinics use electronic health records that pop up alerts when a new prescription might clash with an existing one. Sounds perfect, right? Not quite. Doctors override 90 to 95% of these alerts. Why? Too many false alarms. A system that warns you about every minor interaction becomes noise, not help.But here’s the good news: high-severity alerts-like those warning against combining warfarin and amiodarone-get followed 75% of the time. That means systems work when they’re smart enough to flag only the dangerous stuff. The FDA and ONC are pushing for standardized severity ratings (contraindicated, major, moderate, minor) in all EHRs by 2025. That’s a step forward.
Meanwhile, AI tools like IBM Watson Medication Safety are showing promise. In a 2023 trial at Mayo Clinic, the AI predicted severe interactions with 92.4% accuracy. These tools aren’t replacing doctors-but they’re becoming powerful allies.
When You’re the Patient: What You Can Do Today
You’re not powerless. Here’s what to do the moment you’re prescribed a new drug:- Ask: “Could this interact with anything else I’m taking?” Don’t let them brush you off.
- Request a medication review. Especially if you’ve recently been discharged from the hospital or changed providers. A pharmacist-led review within 72 hours of a new prescription can cut hospital readmissions by over 20%.
- Track your symptoms. Keep a simple journal: date, new med, how you felt that day. Did you feel more tired? Any muscle aches? Dizziness? Bring it to your next visit.
- Don’t self-adjust. If you think a drug isn’t working, don’t double up. If you’re worried about side effects, don’t skip doses. Call your provider. There’s almost always a safer alternative.
Why This Matters More Than Ever
The problem is growing. Nearly half of adults over 65 take five or more medications. The FDA gets 12,000 drug interaction inquiries every year-and that number is rising 25% annually. The Institute of Medicine estimates that following current guidelines could prevent 150,000 to 200,000 serious adverse events in the U.S. each year. That’s not just numbers. That’s people avoiding hospital stays, kidney failure, strokes, or death.And it’s not just about pills. It’s about communication. Only 35% of community pharmacies do full medication reviews. And 42% of patients don’t understand the warnings they’re given. That’s why your role matters. You’re the one who takes the pills. You’re the one who knows how you feel. You’re the one who can ask the question before it’s too late.
Final Thought: Safety Is a Habit, Not a One-Time Check
Managing drug interactions isn’t something you do once when you start a new med. It’s something you do every time your meds change-whether it’s a new prescription, a different dose, or even a new supplement you bought online. Build the habit: update your list, ask questions, listen to your body, and trust your pharmacist. The system isn’t perfect. But you can be the missing piece that keeps you safe.Can over-the-counter pain relievers interact with my prescription drugs?
Yes. Common OTC painkillers like ibuprofen or naproxen can increase bleeding risk when taken with blood thinners like warfarin or aspirin. They can also raise blood pressure in people taking ACE inhibitors or beta-blockers. Even acetaminophen (Tylenol) can stress the liver if you’re on statins, antivirals, or seizure meds. Always check with your pharmacist before taking any OTC drug, even if it’s "just for a headache."
Is it safe to take herbal supplements with my medications?
Many are not. St. John’s Wort is the most dangerous-it cuts the effectiveness of antidepressants, birth control, HIV meds, and immunosuppressants by up to 60%. Garlic, ginkgo, and ginseng can also thin your blood and interfere with surgery or anticoagulants. Even vitamin K can make warfarin less effective. There’s no such thing as a "natural" supplement that’s automatically safe. Always disclose every supplement you take.
What should I do if my doctor prescribes a drug that interacts with one I’m already taking?
Ask if there’s an alternative. For example, if you’re on amlodipine and need a statin, ask if pravastatin or rosuvastatin would work instead-both are less likely to interact. If no alternative exists, ask about dose adjustments and monitoring. For high-risk combos like warfarin and amiodarone, expect weekly INR checks for the first month. Never assume the interaction is "fine" just because your doctor prescribed it. Push for clarity.
How long after starting a new drug should I watch for interactions?
It depends on the drug. For drugs like warfarin or amiodarone, watch closely for the first 3 to 5 days. For statins, muscle pain can show up within 1 to 2 weeks. Some interactions, like those involving CYP3A4 inhibitors, build up slowly over weeks. If you’re on multiple new meds, monitor for 4 to 6 weeks. Keep a symptom log. If anything feels off, call your provider-don’t wait for your next appointment.
Do alcohol and caffeine count as drug interactions?
Absolutely. Alcohol can intensify drowsiness from sedatives, opioids, or antihistamines. It can also damage your liver when taken with acetaminophen or certain antibiotics. Caffeine can raise blood pressure if you’re on beta-blockers, and it can interfere with how some antidepressants are metabolized. Even one or two drinks a day can matter. If you drink alcohol or consume large amounts of caffeine, tell your doctor. They need to know.
Can kidney or liver problems make interactions worse?
Yes. If your kidneys or liver aren’t working well, your body can’t clear drugs the way it should. That means even normal doses can build up to toxic levels. People with an eGFR below 30 mL/min or liver disease face 2.5 to 4 times higher risk of harmful interactions. Always tell your provider about any kidney or liver condition-no matter how mild it seems.
Next Steps: What to Do Right Now
If you’re starting a new medication this week, do this:- Write down every pill, supplement, and OTC drug you take.
- Call your pharmacy and ask them to review your list for interactions.
- Ask your prescriber: "Is this safe with everything else I’m taking?"
- Set a reminder to check in with yourself in 3 days: "Do I feel different? Any new symptoms?"
- Keep your list updated. Add or remove meds as they change.
Medication safety isn’t about memorizing every possible interaction. It’s about building habits that keep you protected. One list. One question. One check-in. That’s how you stop a problem before it starts.







sue spark
15 Dec 2025 at 21:00I started a new blood pressure med last month and didn't think twice about my garlic supplement until my pharmacist called me out. Turns out it was making my INR jump. Never skip the pharmacy review. This post saved me from a hospital trip.