Swallowing seems simple-until it doesn’t. If you’ve ever felt food stick in your chest, or found yourself avoiding solid foods because they just won’t go down, you’re not alone. Thousands of people live with esophageal motility disorders, where the muscles in the esophagus don’t work right. It’s not just about choking. It’s about a broken system that sends food the wrong way-or stops it entirely. And the key to fixing it? Understanding what’s really happening inside, which comes down to two things: dysphagia and manometry.
What Exactly Is Going Wrong in Your Esophagus?
Your esophagus isn’t just a tube. It’s a muscle that contracts in a precise, wave-like motion called peristalsis. Think of it like squeezing a toothpaste tube from the bottom up-food gets pushed smoothly into the stomach. In esophageal motility disorders, that wave gets messy. Sometimes it’s too weak. Sometimes it’s too strong. Sometimes it doesn’t happen at all. And the lower esophageal sphincter (LES), the valve between your esophagus and stomach, might not open when it should.The most common symptom? Dysphagia. Not just trouble swallowing solids-later, even liquids. Many people think it’s acid reflux, so they take PPIs for years. But if your esophagus isn’t moving right, antacids won’t help. You’ll keep regurgitating food, losing weight, or getting chest pain that feels like a heart attack. In fact, 40-50% of people with diffuse esophageal spasm end up in the ER thinking they’re having cardiac issues.
These disorders aren’t rare. While achalasia affects about 1 in 100,000 people each year, up to 10% of people with dysphagia have some form of motility problem. And they’re often missed. A survey of over 1,200 patients found that nearly 70% waited 2 to 5 years for a correct diagnosis. Some saw three or more doctors before someone finally ordered the right test.
Why Manometry Is the Gold Standard
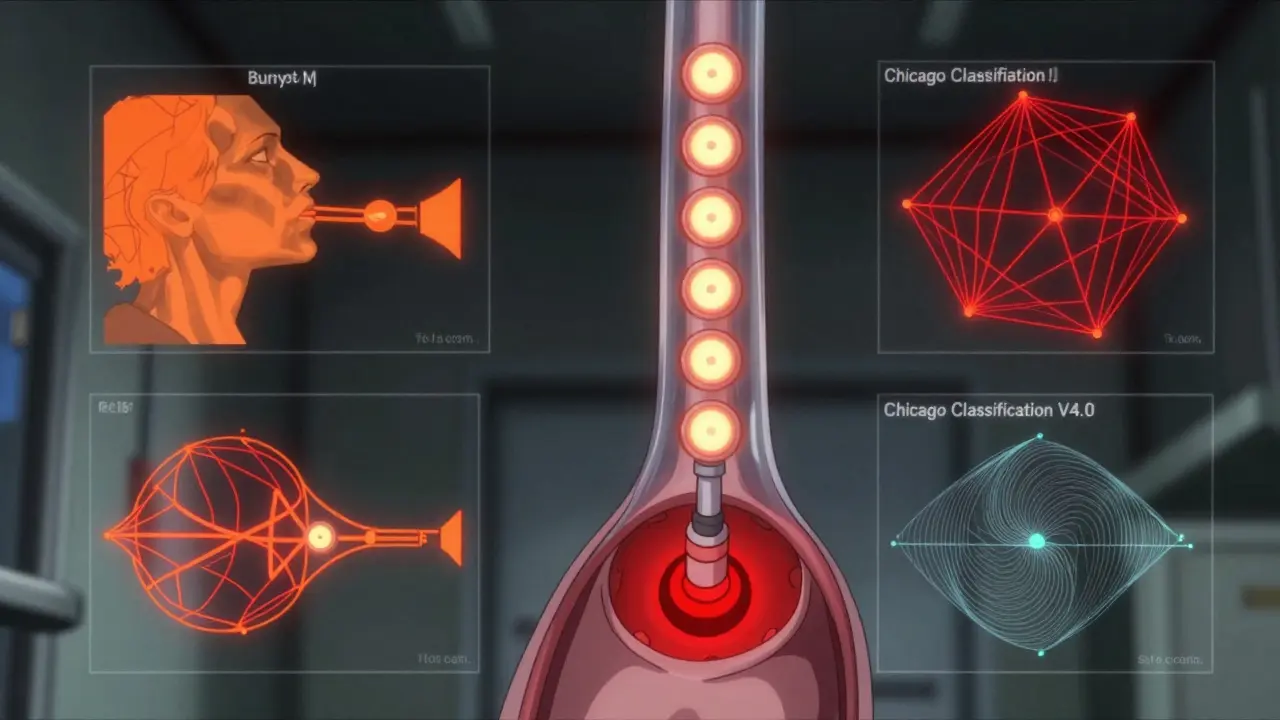
You can’t see muscle contractions with an endoscope. You can’t measure pressure with an X-ray. That’s why esophageal manometry-especially high-resolution manometry (HRM)-is the gold standard. It’s not glamorous. You swallow a thin, flexible tube with 36 tiny pressure sensors spaced every centimeter. As you take sips of water, the machine maps every contraction in real time.Before the 2000s, doctors used older manometry with just a few sensors. It was like trying to map a highway with three checkpoints. HRM gives you a full satellite view. It can spot the difference between a weak squeeze and a violent spasm. It can tell if the LES is stuck shut or too tight. And it’s accurate-96% for diagnosing achalasia, compared to 78% for a barium swallow.
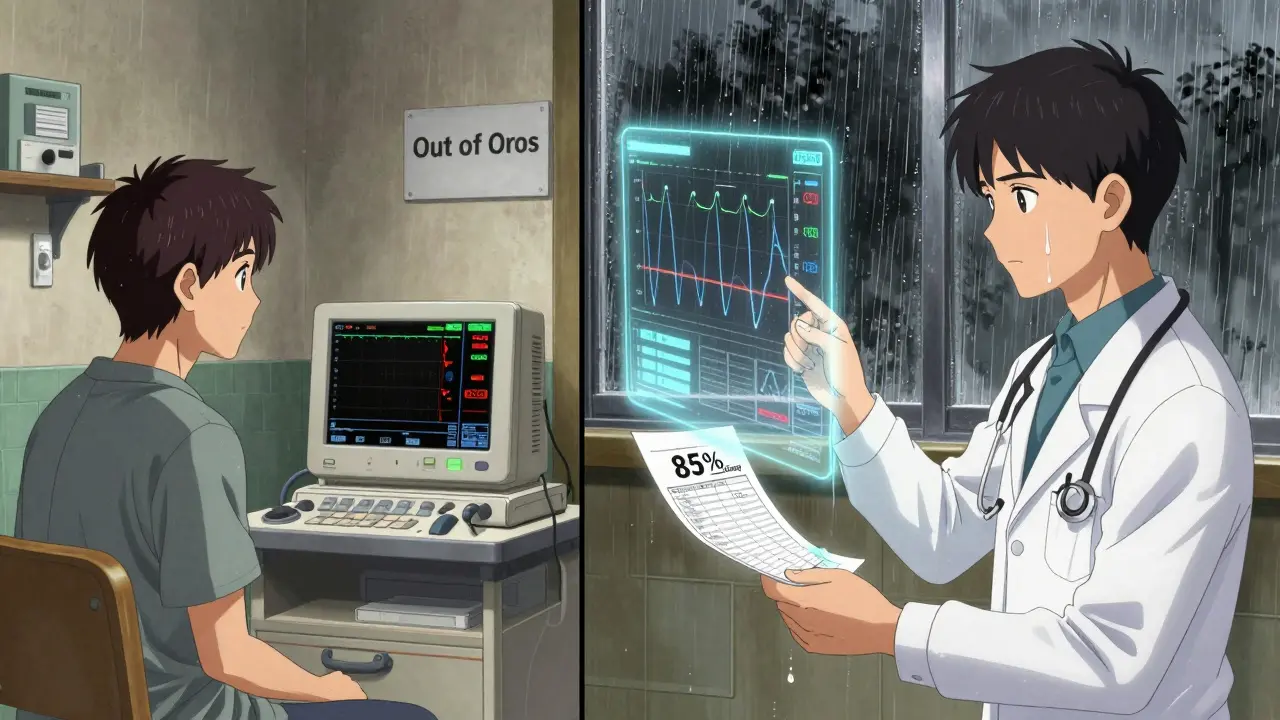
The breakthrough came with the Chicago Classification. First launched in 2008 and updated in 2023 (v4.0), it turned manometry from an art into a science. Before, two doctors might disagree on what they saw. Now, with clear criteria, agreement jumps to 85%. That’s huge. It means fewer misdiagnoses and better treatment.
The Main Disorders and How They Show Up
Not all motility disorders are the same. Here’s what the data shows:- Achalasia (the most studied): The LES won’t relax, and the esophagus loses its ability to squeeze. There are three types: Type I (no contractions, 20% of cases), Type II (whole esophagus pressurizes like a balloon, 70%), and Type III (spasms, 10%). Patients often lose 15-20 pounds and regurgitate food.
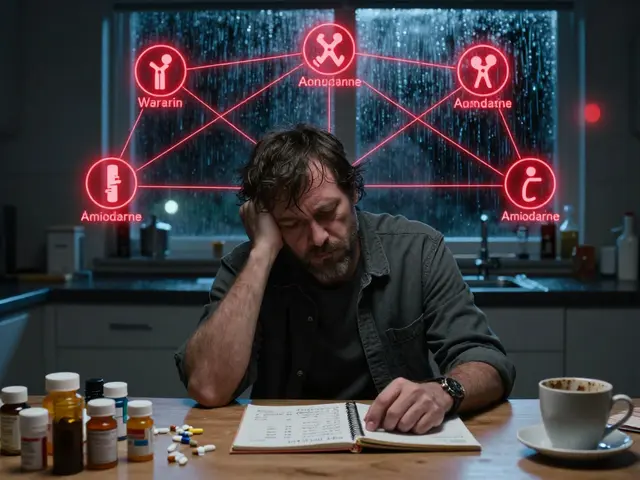
- Diffuse Esophageal Spasm (DES): Uncoordinated, chaotic contractions. Causes chest pain that mimics a heart attack. Often misdiagnosed as angina.
- Nutcracker Esophagus: Contractions are too strong-over 180 mmHg. Painful, but doesn’t usually block food.
- Jackhammer Esophagus: Extreme contractions with a pressure over 5,000 mmHg•s•cm. Patients describe it as “a hammer hitting their chest.”
- Hypertensive LES: The valve pressure stays above 26 mmHg. Can cause dysphagia without other contractions.
- Secondary disorders: Often tied to diseases like scleroderma. Up to 80% of scleroderma patients develop esophageal muscle damage from fibrosis.
These aren’t just labels. They guide treatment. You wouldn’t treat jackhammer the same way you’d treat achalasia.
How Diagnosis Changes Everything
The standard path starts with an upper endoscopy to rule out tumors or strictures. If nothing’s blocking the tube, the next step is HRM. That’s when the real story emerges.Take the case of a 58-year-old woman who’d been on PPIs for eight years. She still couldn’t swallow bread. Her endoscopy looked fine. HRM showed jackhammer esophagus. Once she stopped acid blockers and started targeted therapy, her symptoms vanished. That’s not rare. Dr. Kristle Lee Lynch from the Perelman School of Medicine says, “Many patients are treated for GERD for years while their real problem goes untreated.”
Another tool gaining traction is the Multiple Rapid Swallows (MRS) test. During HRM, you swallow five quick sips. A healthy esophagus responds by suppressing contractions and relaxing the LES. If it doesn’t? That’s a red flag for achalasia or severe motility failure.
And it’s not just pressure. New tech like EndoFLIP measures how stretchy the esophagus is. It’s especially useful for patients with esophagogastric junction outflow obstruction (EGJOO)-a new category in Chicago v4.0. This helps doctors decide whether surgery or dilation is the better option.
Treatment: From Surgery to New Tech
Treatment depends on the diagnosis. For achalasia, the two main options are:- Laparoscopic Heller myotomy (LHM): A surgeon cuts the tight LES muscle. Success rate: 85-90% at five years. But it can lead to reflux in about 30% of cases.
- Peroral endoscopic myotomy (POEM): A scope goes in through the mouth, cuts the muscle from the inside. Just as effective as LHM, but higher reflux rates-up to 44% at two years.
Pneumatic dilation (inflating a balloon to stretch the LES) works for 70-80% of patients at first. But 25-35% need repeat procedures within five years. It’s less invasive than surgery, but not always permanent.
Newer options are emerging. The LINX device-a ring of magnetic beads around the LES-helps some patients with preserved peristalsis. And wireless manometry capsules (like SmartPill) let you test motility at home over 24 hours. They’re not perfect, but they correlate at 85% with traditional HRM. That’s a game-changer for people who can’t get to a specialty center.
And yes, AI is coming. Early studies show AI tools can identify achalasia patterns with 92% accuracy-better than some human interpreters without formal training. This could help bring expert-level diagnosis to smaller hospitals.
Why So Many Patients Are Still Left Behind
Here’s the hard truth: HRM machines cost $50,000 to $75,000. Training takes 6-12 months. Only 35% of community hospitals in the U.S. have them. In low-income countries? Less than 10%. That means many people never get tested.And even when they are, misinterpretation is common. A study found that without Chicago Classification training, inter-observer agreement was only 65%. After training? It jumped to 88%. That’s why resources like the Esophageal Disorders Society’s online course-completed by over 1,200 doctors in 2023-are so vital.
Patients report better experiences when they’re prepared. One survey found satisfaction with HRM jumped from 45% to 78% when doctors explained the procedure clearly beforehand. No one likes a tube down their throat. But knowing why it’s needed? That makes all the difference.
What’s Next?
The global market for esophageal diagnostics is growing fast-projected to hit $410 million by 2028. More awareness, better tech, and clearer guidelines mean more people will get diagnosed. But access remains uneven. Rural areas, low-income regions, and underserved populations still lag far behind.The future lies in combining HRM with impedance monitoring, AI-assisted interpretation, and less invasive tools. But the biggest change won’t be technological-it’ll be cultural. We need to stop assuming dysphagia is just GERD. We need to listen when patients say, “I’ve tried everything, and nothing helps.” And we need to make sure the right test is offered-not just the easiest one.










Tatiana Barbosa
7 Feb 2026 at 08:02Finally, someone put this into terms I can understand. I’ve been living with dysphagia for years and was told it was ‘just acid reflux’ until I demanded manometry. That HRM test? Life-changing. The way they map every contraction? It’s like seeing the ghost in the machine. No more guessing. No more PPIs that did nothing. I wish every GI doc had this clarity.