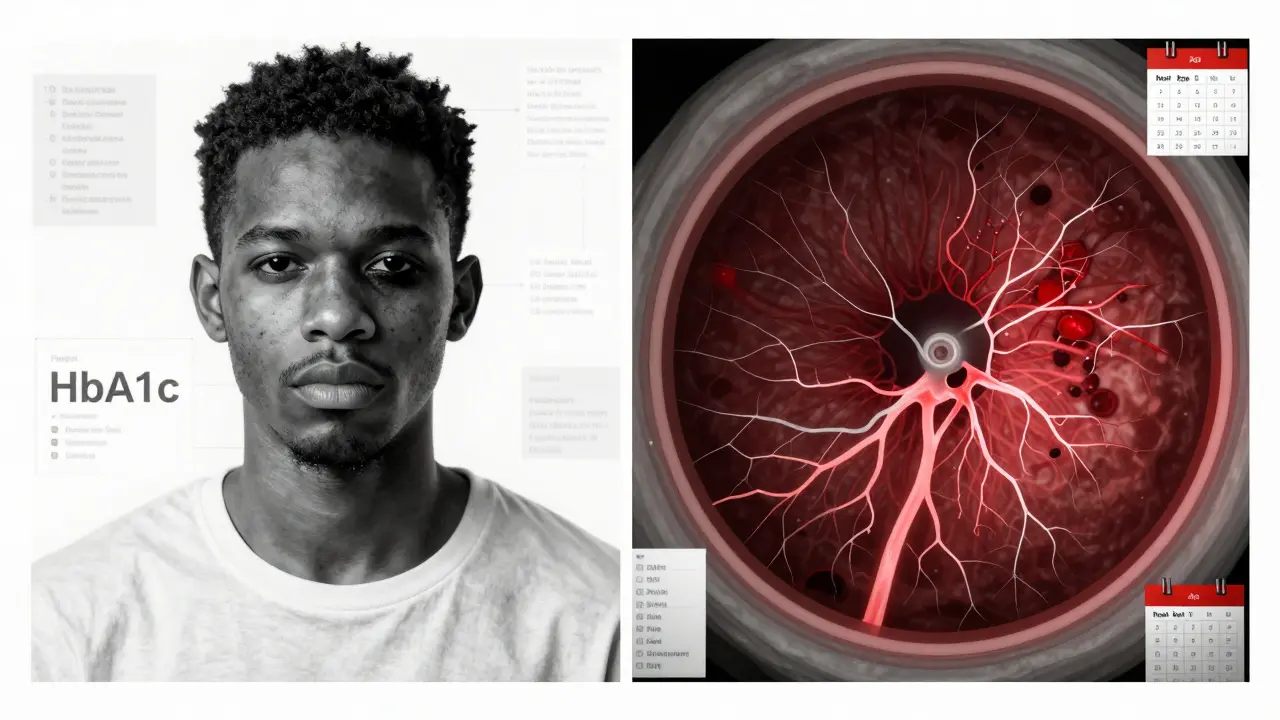
One in three people with diabetes will develop vision problems. And here’s the scary part: diabetic eye screening can stop 90% of those cases before they ruin your sight. Yet, only about 60% of people with diabetes get the checkups they need. Why? It’s not that they don’t care. It’s often because the system is broken-long waits, distant clinics, painful eye drops, and confusing advice.
When Should You Get Your First Diabetic Eye Screening?
If you have type 1 diabetes, your first eye exam should happen within five years after diagnosis. That’s not a suggestion-it’s a medical rule backed by decades of research. For type 2 diabetes, it’s different. You get screened right away, at diagnosis. Why? Because many people have had undiagnosed diabetes for years before they’re told they have it. By then, damage might already be starting.
That first exam isn’t just a quick glance. It’s a full dilated eye exam. Pupils are widened with drops so the doctor can see every blood vessel, every tiny leak, every early sign of swelling in the retina. It takes about 20 minutes. You’ll be blurry for hours afterward. You can’t drive. You might miss your kid’s soccer game. But it’s worth it.
How Often Should You Be Screened After That?
It’s not one-size-fits-all. Your frequency depends on what the doctor finds-and how well your blood sugar is controlled.
- If your eyes are completely healthy and your HbA1c is under 7%, you might only need a checkup every 1-2 years.
- If you have mild retinopathy, you’ll need to come back every 6-12 months.
- If your condition is worsening or you have swelling in the macula (diabetic macular edema), you’ll need to be seen every 2-4 months.
- If you’re in the advanced stages-new blood vessels growing, bleeding in the eye-you’ll need to be seen every month or more.
The American Diabetes Association updated these guidelines in January 2025. They’re clear: skipping screenings is dangerous. The Wisconsin study showed people who miss their annual exams are 23 times more likely to lose vision. That’s not a risk you take with your eyes.
What Is Teleophthalmology, and Why Does It Matter?
Imagine getting your eye screening done during your regular diabetes checkup-no extra trip, no dilation drops, no waiting weeks for an appointment. That’s teleophthalmology.
It works like this: a non-specialist takes a photo of your retina using a special camera. The image gets sent to a remote eye doctor who reads it. In some places, AI software checks the image first, flagging anything suspicious. The whole process takes five minutes.
It’s not magic. It’s science. The FDA-approved system LumineticsCore (formerly IDx-DR) detects serious retinopathy with 87% accuracy. In rural India, a program screened 15,000 people with 98.5% agreement with in-person specialists. In the U.S. Veterans Health system, screening rates jumped 32% after they rolled out teleophthalmology.
For people in remote areas, it’s life-changing. In rural Australia, where the nearest ophthalmologist might be 200 kilometers away, teleophthalmology means you don’t have to miss work, pay for gas, or beg for a ride just to protect your vision.

Why Isn’t Everyone Using It?
Because it’s not perfect.
Retinal photos don’t catch everything. They can’t detect cataracts, glaucoma, or dry eye. They can’t replace a full exam if something looks off. And they need infrastructure: a good camera, a stable internet connection, trained staff, and a system to send and store images securely.
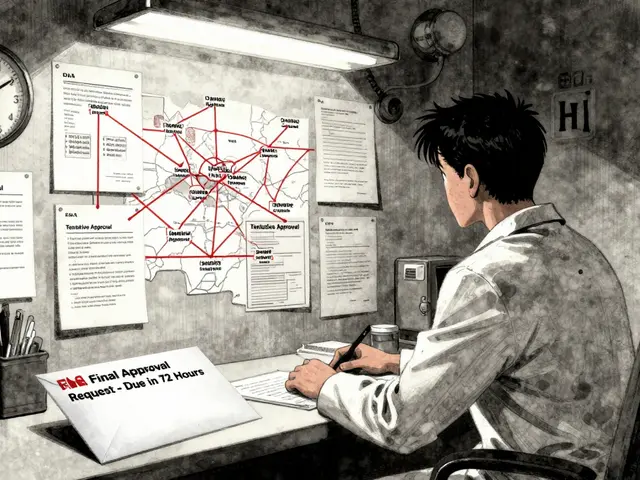
Startup costs? Around $28,500 per site. That’s a lot for a small clinic. Insurance doesn’t always pay for it-only 63% of private insurers cover teleophthalmology in 2024. And there’s a hidden inequality: clinics serving low-income patients are 47% less likely to have the technology, even though those patients are at higher risk.
There’s also a trust issue. Some patients don’t believe a photo can replace a real doctor. One Reddit user wrote, “My kid’s birthday party was ruined by dilation drops. We need non-invasive options.” Teleophthalmology answers that. No drops. No blur. Just a quick flash.
How Do You Make Sure You Get Screened?
Don’t wait for your doctor to remind you. Most don’t. A 2024 University of Michigan study found 58% of diabetes patients thought controlling blood sugar alone was enough to protect their eyes. It’s not. You still need the scan.
Here’s what works:
- Set a recurring calendar reminder for your annual eye exam-mark it the same day as your HbA1c test.
- Ask your primary care provider if your clinic offers teleophthalmology. If not, ask why.
- If you’re in a rural area, check with your local health department. Many now partner with teleophthalmology networks.
- Keep your records. If you get screened at a pharmacy or community clinic, make sure the results go to your diabetes doctor.
Kaiser Permanente cut missed appointments by 27% using automated SMS reminders sent 21, 14, and 7 days before the visit. You can do the same.
What’s Changing in 2025?
The rules are shifting. Medicare now accepts teleophthalmology screenings as meeting the official quality measure (CMS Quality ID #117). That means doctors get paid for doing it. That’s a big deal.
AI is getting smarter. In 2022, only 8% of Medicare diabetes screenings used AI. Now it’s 22%. That number will keep climbing.
And researchers are working on something even bigger: personalized screening. Instead of everyone getting checked every year, future systems might use 17 different factors-blood sugar trends, blood pressure, cholesterol, genetics, even how long you’ve had diabetes-to figure out if you can wait two or even three years between scans. The T1D Exchange is already testing this in clinical trials.
But here’s the catch: these advances won’t help if they only reach people who already have access. The real challenge isn’t the technology. It’s equity.
What If You’re Not Sure You Need It?
Here’s the truth: if you have diabetes, you need this screening. No exceptions. Even if you feel fine. Even if your vision is perfect. Diabetic retinopathy doesn’t hurt. It doesn’t blur your sight until it’s too late.
It’s not optional. It’s not a luxury. It’s as essential as checking your blood sugar or taking your insulin. Your eyes don’t have a pain signal. That’s why we need the camera.
And if you’ve been skipping screenings because of cost, distance, or discomfort-there’s a better way now. Teleophthalmology is here. It’s safe. It’s proven. And it’s working.
Don’t wait for your vision to go. Take five minutes this week. Call your doctor. Ask: Do you offer teleophthalmology? If not, ask why. And then make sure you get screened-on time, every time.
How often should someone with type 2 diabetes get an eye exam?
Most people with type 2 diabetes should get a dilated eye exam at diagnosis, and then annually. If your eyes are healthy and your HbA1c is under 7% for two years in a row, your doctor may suggest every 1-2 years. But if you have any signs of retinopathy, you’ll need to be seen more often-every 6 to 12 months, or even every few months if it’s worsening.
Can teleophthalmology replace a full eye exam?
No, not completely. Teleophthalmology uses retinal photos to detect diabetic retinopathy and macular edema, which are the most common causes of vision loss in diabetes. But it can’t detect other eye problems like glaucoma, cataracts, or dry eye. That’s why the first exam should always be a full dilated checkup with an eye specialist. After that, teleophthalmology can be a reliable follow-up tool-especially in areas with few specialists.
Is AI eye screening accurate?
Yes, the FDA-approved systems like LumineticsCore are highly accurate. In clinical trials, they detected more than mild diabetic retinopathy with 87.2% sensitivity and 90.7% specificity. That means they catch almost all serious cases and rarely give false alarms. They’re not perfect, but they’re reliable enough to be used as a screening tool-especially when a human expert reviews the flagged cases.
Why do some people miss their diabetic eye screenings?
The top reasons are transportation issues (68% of patients cite this), discomfort from pupil-dilating drops (42%), and lack of awareness that it’s needed even if vision is fine. Many also don’t know where to go or think their regular doctor will handle it. In rural areas, the nearest specialist might be hours away. Teleophthalmology helps solve these problems by bringing the screening to the patient’s regular diabetes visit.
Does Medicare cover teleophthalmology for diabetic eye screening?
Yes. As of November 2024, Medicare accepts teleophthalmology screenings as meeting the requirements for Quality Measure #117. That means providers are reimbursed for performing them. Many private insurers still don’t cover it fully-only 63% did in 2024-but coverage is improving as evidence grows.
Can I skip my eye exam if my blood sugar is under control?
No. Even with perfect HbA1c levels, you can still develop diabetic retinopathy. A 2023 study showed African American patients developed advanced eye disease 2.3 years earlier than white patients with the same blood sugar control. That’s why screening isn’t optional-it’s essential, no matter how well you manage your diabetes.







Thomas Anderson
15 Dec 2025 at 08:36Just got my screening last week-no dilation, just a quick flash with the camera. Took 5 minutes. My doc said I’m good for another year. No more driving blind after appointments. Game changer.