Every time you pick up a new prescription, there’s a label on the bottle that holds the keys to taking your medicine safely. But if you’ve ever stared at it and thought, What does this even mean? - you’re not alone. Around 79% of patients misread at least one part of their prescription label, according to a major NIH study. That’s not just confusing - it’s dangerous. Misunderstanding your label can lead to overdoses, missed doses, or harmful side effects. The good news? Learning how to read it is simple. You don’t need a medical degree. You just need to know what to look for.
Start with Your Name
The very first thing on the label should be your full name. Not just your first name. Not a nickname. Your legal first and last name. This isn’t just paperwork - it’s a safety check. Pharmacies fill hundreds of prescriptions a day. Someone else might be on the same medication, or even have a similar-sounding name. If your name doesn’t match exactly, don’t take the pills. Call the pharmacy right away. A mismatch here is rare, but when it happens, it can be life-threatening.
Medication Name: Brand vs. Generic
You’ll see two names here. One is the brand name - like Lipitor. The other is the generic name - atorvastatin. In Australia and Canada, the generic name usually comes first. In the U.S., it’s often listed second. Either way, both names mean the same thing. The brand name is what the drug company calls it. The generic name is the actual medicine. If your doctor switches you from brand to generic, your pills might look different, but they work the same. Always check that the name on the label matches what your doctor told you. If it doesn’t, ask why.
Prescription Number (Rx#)
This is a unique code, usually starting with “Rx” followed by numbers and letters. It’s not just for the pharmacy’s records. This number is your shortcut when you need to refill or have a question. If you call the pharmacy and say, “I have a question about my prescription,” they’ll ask for your name. But if you give them your Rx#, they can pull up your exact bottle in seconds. Keep this number handy - write it on your phone or in your notes. It saves time and avoids mix-ups.
Who Prescribed It?
Underneath the medication name, you’ll see the name of the person who wrote the prescription. It could be your doctor, a nurse practitioner, a dentist, or even a vet if it’s for an animal. This tells you who ordered it. If you didn’t see this provider recently, or if you’re unsure why you’re taking this medicine, call them. Sometimes prescriptions get mixed up during transfers between clinics. Knowing who ordered it helps you confirm it’s the right one.
Strength and Dosage
This part tells you how much medicine is in each pill, tablet, or milliliter. It might say “20 mg” or “500 mg.” That’s the strength. Then, the instructions tell you how many to take. “Take one tablet by mouth twice daily” means two pills a day - not four. A common mistake? Thinking “twice daily” means every two hours. That’s wrong. Twice daily means morning and night, roughly 12 hours apart. If the label says “every 8 hours,” that’s different - you’d need to set alarms. Don’t guess. If you’re unsure, ask your pharmacist to explain it in plain language.

Quantity and Discard Date
The quantity tells you how many pills or how much liquid you got. If you were supposed to get 30 tablets and you got 60, double-check. That could be a mistake. The discard date - sometimes called the expiration date - is critical. Most prescriptions are good for one year from the day they were filled. After that, the medicine may not work as well. Some, like insulin or eye drops, expire sooner. Never take medicine past this date. Even if it looks fine, it might not be safe.
Refill Information
Look for a line that says “Refills: 2” or “No refills.” This tells you how many more times you can get the same prescription without a new doctor’s note. If you run out and try to refill, and it says “No refills,” you’ll need to book an appointment. Don’t wait until the last pill. Plan ahead. If you’re on a long-term medication, ask if you can get a 90-day supply. It saves trips and often costs less.
Auxiliary Labels: The Small Print That Matters
These are the little stickers or printed notes on the bottle. Things like:
- “Take with food” - to avoid stomach upset
- “Avoid sunlight” - because the medicine can make your skin burn easily
- “Refrigerate” - keep it cold, don’t leave it on the counter
- “May cause drowsiness” - don’t drive or operate machines
- “Do not drink alcohol” - mixing can be dangerous
These aren’t suggestions. They’re warnings. Skipping them can cause real harm. If you see one you don’t understand, ask your pharmacist to explain it. Don’t assume.
Drug Identification Numbers: DIN or NDC
In Australia and Canada, you’ll see a DIN - Drug Identification Number. It’s an 8-digit code. In the U.S., it’s the NDC - National Drug Code. This number is unique to that exact medicine, strength, and manufacturer. It’s not for you to remember, but it’s there so the pharmacy and regulators can track it. If you ever need to report a problem with the medicine - like a bad reaction - this number helps them find the exact batch.
Pharmacy Contact Info
At the bottom, you’ll find the pharmacy’s name, address, and phone number. Keep this visible. If you have a question - even a small one - call them. Pharmacists are trained to explain labels. They’re not there just to hand out pills. They’re your safety net. If you’re confused, they’d rather you call than risk taking it wrong. Many pharmacies also offer free medication reviews. Ask if they have one available.
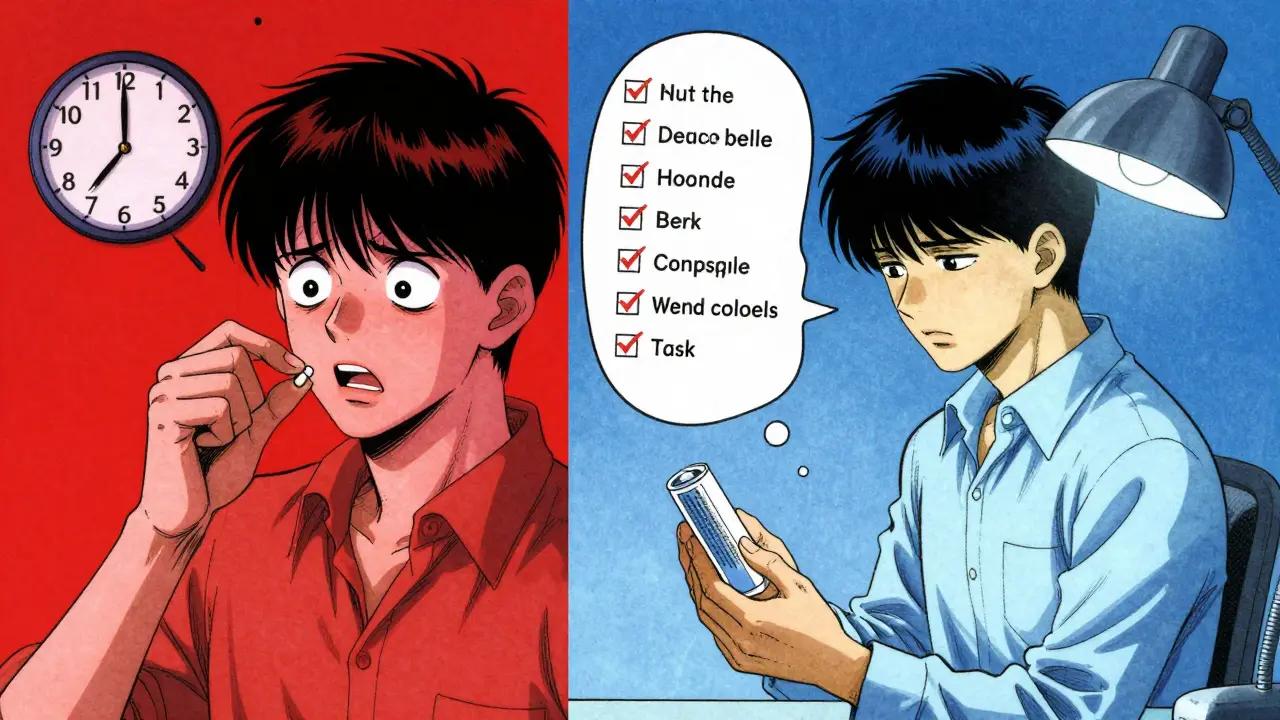
Seven Checks Before You Take It
Before you swallow any pill, do this quick mental checklist:
- Is my name on the label? (Exact match)
- Is the medication name correct? (Brand or generic)
- Does the strength match what I was told? (20 mg, not 40 mg)
- Do I understand the instructions? (“Twice daily” = morning and night)
- Are there any auxiliary warnings? (Food, sun, alcohol, etc.)
- Is the discard date still valid? (Not expired)
- Do I have the pharmacy’s number? (So I can call if unsure)
Taking two minutes to do this every time you get a new prescription cuts your risk of a medication error dramatically. It’s not about being careful - it’s about being smart.
Why This Matters More Than You Think
Medication errors are one of the leading causes of preventable harm in healthcare. In the U.S., they contribute to 1.5 million injuries each year. In Australia, the numbers are similar. Most of these errors happen because someone didn’t understand their label. A 2022 study found that patients who clearly understood their prescriptions were 28% more likely to take their medicine as directed. That means fewer hospital visits, fewer side effects, and better health outcomes. This isn’t just about following rules - it’s about protecting your body.
What to Do If You’re Still Confused
Don’t guess. Don’t assume. Don’t wait until you feel something weird. Go back to the pharmacy. Ask the pharmacist to walk you through the label. Many now offer free 5-minute consultations. Bring your list of all medications - even supplements. Some pharmacies have apps with video instructions in multiple languages. Others offer printed guides in large print. If you have trouble reading, ask for help. There’s no shame in it. The system is designed to make this hard. Your job is to make it work for you.
What’s Coming Next
Pharmacies are starting to use QR codes on labels. Scan it, and you’ll get a short video in your language showing how to take the medicine. Some are even adding voice instructions. By 2025, most Australian pharmacies will offer digital label options through their apps. But until then, the paper label is still your main tool. Learn to read it. Master it. It’s one of the simplest, most powerful things you can do for your health.
What if my prescription label looks different from last time?
It’s normal for labels to change slightly - new pharmacy, different printer, updated guidelines. But if the medication name, strength, or instructions are different from what your doctor prescribed, call the pharmacy immediately. Also check if the pill shape or color changed. If you’re unsure, ask for a medication review. Never assume it’s the same.
Can I take my medicine with food if it doesn’t say so?
Only if it’s safe. Some medicines work better on an empty stomach. Others can upset your stomach if taken without food. If the label doesn’t say anything, call your pharmacist. They’ll know if food affects absorption or side effects. Never guess - even if you’ve taken it with food before.
What should I do if I miss a dose?
Check the label first. Some instructions say, “Take as soon as you remember.” Others say, “Skip it and wait for the next dose.” Never double up unless told to. If the label doesn’t say, call your pharmacist. Missing one dose usually won’t hurt - but doubling up can be dangerous.
Why do some labels say “Take with food” and others don’t?
It depends on how the medicine works. Some need food to be absorbed properly. Others can cause nausea if taken on an empty stomach. Some are fine either way. The label tells you what the manufacturer tested. If it doesn’t say anything, it usually means food doesn’t affect it. But if you’re unsure, ask your pharmacist - they can tell you what’s safe.
Can I trust the expiration date on my prescription?
Yes - but only if it’s the date on the label. That’s the date the pharmacy set based on when they filled it. Most prescriptions expire one year after dispensing. Don’t rely on the manufacturer’s printed date - it’s often years in the future. The pharmacy’s date is the one that matters. If it’s expired, don’t use it. Get a new one.










Write a comment