When two or more drugs are combined into a single pill or formulation, the goal is simple: better results with fewer pills. But behind that simplicity lies a complex challenge-therapeutic equivalence. Just because two combination products have the same active ingredients doesn’t mean they’re interchangeable without risk. This is especially true when doses differ, formulations change, or patients switch between brands and generics.
What Therapeutic Equivalence Really Means
Therapeutic equivalence isn’t about two drugs being "similar." It’s about being clinically identical. The U.S. FDA defines it strictly: two products must contain the same active ingredients, in the same amounts, in the same dosage form, and delivered the same way. If they meet all these criteria and pass bioequivalence testing, they get an "A" rating in the FDA’s Orange Book. Over 14,000 drug products have been rated this way, and 95% of them are rated "A." That sounds reassuring-until you dig deeper. The catch? Therapeutic equivalence doesn’t guarantee identical results in every patient. It means the average patient will respond the same. But what about the person whose body metabolizes drugs differently? Or the one on multiple medications where tiny changes in absorption matter?Dose Equivalence in Combination Products
Combination products like amlodipine/benazepril or tramadol/acetaminophen aren’t just mixtures-they’re interactions. The effect isn’t always additive. Sometimes, one drug boosts the other. In preclinical studies, tramadol and acetaminophen together reduced pain more than either drug alone. That’s synergy. But when you switch from a brand to a generic, even if the active ingredients match, the way those ingredients are released can change. Take amlodipine/benazepril. One generic might use croscarmellose sodium as a disintegrant. Another uses sodium starch glycolate. Sounds minor. But in a patient with slow gastric emptying or kidney disease, that difference can alter how quickly the drugs enter the bloodstream. One pharmacist reported three dosing errors in six months just from switching between generics of this combo. No one changed the prescription. The pharmacy just filled it with a different manufacturer’s version.Narrow Therapeutic Index Drugs Are the Real Danger
Some drugs have a razor-thin line between working and causing harm. These are called narrow therapeutic index (NTI) drugs. Warfarin, levothyroxine, phenytoin-they’re all in this group. When they’re part of a combination, the risk multiplies. A 2018 study found that 12% of patients switching between different levothyroxine generics-even though they were all rated "A"-had adverse events. Their TSH levels jumped. Some felt fatigued. Others had heart palpitations. The FDA requires a tighter bioequivalence range for NTI drugs: 90-111% instead of the usual 80-125%. But even that isn’t foolproof. When levothyroxine is combined with another drug-say, a statin or an antidepressant-the interaction can mask or amplify those small absorption differences. The result? A patient who was stable for years suddenly feels off. Their doctor thinks it’s their thyroid, not the pill they just switched to.
Why Generic Substitutions Go Wrong
The system is designed to save money. And it does. Generic drugs saved the U.S. healthcare system $1.7 trillion over the past decade. But savings shouldn’t come at the cost of safety. Here’s how it breaks down:- 90% of prescriptions are filled with generics. That’s good.
- 18% of those generics are combination products. That’s growing fast.
- But only 72% of psychiatric combination products are rated "A"-compared to 98% of statin combos. Why? Because psychiatric drugs have complex absorption patterns and brain effects that are harder to replicate.
What Pharmacists and Clinicians Must Do
The FDA gives a three-step checklist for therapeutic equivalence:- Confirm the active ingredients match exactly.
- Verify the dosage form and route are identical.
- Check the Orange Book for the TE code.
- Use standardized conversion tables for NTI combinations-don’t guess.
- Scan barcodes on every generic substitution. It flags if the product is from a different manufacturer.
- Monitor high-risk patients for 72 hours after switching. Check labs. Ask how they feel.
- Don’t assume "A" rating = always safe. Some "A" rated products have different release profiles.
What’s Changing in 2025
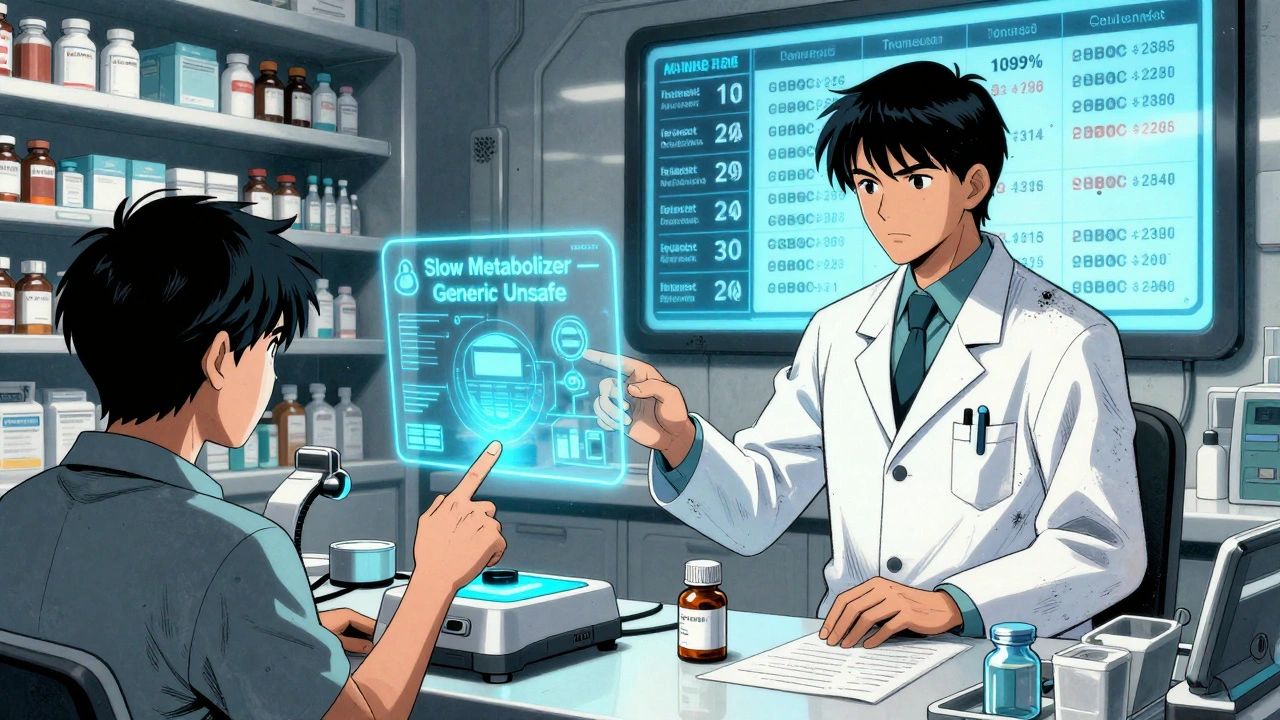
The FDA is moving beyond simple bioequivalence. In early 2023, they released draft guidance on complex combination products-those where the dose-response isn’t linear. One example: a drug that works well at low doses but loses effectiveness or becomes toxic at higher doses. These are common in psychiatric and pain meds. They’re also testing machine learning models that predict which generic substitutions might cause problems. Early tests got 89% accuracy. That means in the near future, a pharmacist might get a warning: "This generic version of this combo has a 72% chance of altering absorption in patients with renal impairment." Meanwhile, the European Medicines Agency requires extra in-vivo studies for fixed-dose combos where components absorb differently. The U.S. might follow.The Future: Personalized Equivalence
By 2030, the NIH predicts 30% of therapeutic equivalence decisions will include pharmacogenomic data. That means your genes will help determine if a generic is safe for you. Imagine this: Your doctor prescribes a combo drug. Before filling it, your pharmacy runs a quick genetic test. It shows you’re a slow metabolizer of one component. The system flags that the generic version you’re being offered might build up to toxic levels. You get the brand. Or a different combo. No guesswork. It’s not science fiction. It’s coming.Bottom Line: Equivalence Isn’t Always Equal
Therapeutic equivalence is a powerful tool. It saves money. It expands access. But it’s not magic. Different doses in combinations aren’t just numbers on a label-they’re signals in the body. A 5% change in absorption can mean the difference between control and crisis. If you’re a patient: Ask if your combo drug is a brand or generic. If you feel different after a switch, speak up. Get your levels checked. If you’re a provider: Don’t assume "A" means safe. Know your NTI drugs. Use the Orange Book. Track your patients after substitutions. If you’re a pharmacist: Scan. Monitor. Educate. Don’t let cost savings override safety. Therapeutic equivalence is about trust. But trust should be earned-not assumed.What does an "A" rating in the FDA Orange Book mean?
An "A" rating means the drug product has been evaluated by the FDA and is considered therapeutically equivalent to the reference listed drug. It contains the same active ingredients, dosage form, strength, route of administration, and meets bioequivalence standards. This allows pharmacists to substitute it without a prescriber’s approval.
Can two combination drugs with the same active ingredients still not be interchangeable?
Yes. Even if two combination products have identical active ingredients and doses, differences in inactive ingredients, release mechanisms, or manufacturing processes can affect how the drugs are absorbed. This is especially risky with narrow therapeutic index drugs like warfarin or levothyroxine. A product may have an "A" rating but still cause clinical changes in sensitive patients.
Why are NTI drugs more dangerous in combination products?
NTI drugs have a very small margin between an effective dose and a toxic one. When combined with another drug, even minor differences in absorption or metabolism can push levels into the toxic range. For example, switching a patient from one generic to another of a levothyroxine/antidepressant combo could cause thyroid hormone levels to spike or drop, leading to heart issues or severe fatigue.
How can pharmacists reduce errors when substituting combination drugs?
Pharmacists can reduce errors by using barcode scanning to track manufacturer changes, maintaining a 72-hour monitoring window for high-risk patients, consulting standardized conversion tables for NTI combinations, and documenting all substitutions in the patient’s record. Staff training on therapeutic equivalence nuances also reduces errors by over 60% in health systems that implement it.
Are all generic combination drugs safe to substitute?
Not always. While most are safe, some combination generics-especially those for psychiatric conditions or NTI drugs-have higher rates of clinical variability. The FDA rates 98% of statin combinations as equivalent, but only 72% of psychiatric combinations. Always check the Orange Book, monitor patients, and never assume equivalence equals identical outcomes.
What’s the biggest risk in switching combination drug brands?
The biggest risk is assuming that identical active ingredients mean identical effects. Subtle differences in how the drug is released or absorbed-due to inactive ingredients or manufacturing-can lead to treatment failure or adverse events. This is especially true for patients on multiple meds, the elderly, or those with kidney or liver issues. The FDA’s approval doesn’t guarantee safety in every individual.










Louis Llaine
6 Dec 2025 at 20:32So let me get this straight-we’re spending billions on generics to save money, but now we’re supposed to micro-manage every pill swap because some guy in a lab in Ohio used a different filler? 🤡