Breathing Disorder Risk Assessment
This tool helps you evaluate your risk for breathing disorders such as asthma, COPD, or sleep apnea based on common symptoms and risk factors. It encourages early detection which is crucial for effective treatment.
Check off any symptoms you experience regularly:
Additional risk factors:
Imagine struggling for air while walking to the bus stop, only to think it’s just a bad day. For millions, that’s a daily reality - but it doesn’t have to be. Catching a breathing problem early can turn a life‑threatening situation into a manageable routine.
What counts as a breathing disorder?
Breathing disorders are conditions that impair the normal flow of air into and out of the lungs. They range from the well‑known asthma attacks to the silent night‑time pauses of sleep apnea. While each disease has its quirks, they all share one glaring weakness: the longer they go undetected, the harder they are to treat.
Why catching it early matters
Early detection does more than just ease symptoms - it preserves lung tissue, reduces medication dosages, and cuts down hospital visits. A study from the Australian Institute of Health (2024) found that patients diagnosed with asthma before age 12 had a 35% lower risk of developing severe COPD later in life. In plain terms, spotting the problem early can keep you breathing easy for decades.
Common culprits and how they differ
| Disorder | Typical Onset | Main Symptom | Standard Test |
|---|---|---|---|
| Asthma chronic airway inflammation | Childhood to early adulthood | Wheezing, shortness of breath | Spirometry |
| COPD progressive airflow limitation | Usually after 40, often linked to smoking | Persistent cough, reduced exercise tolerance | Pulse oximetry, spirometry |
| Sleep apnea repeated airway collapse during sleep | Adulthood, higher in overweight individuals | Loud snoring, daytime fatigue | Polysomnography |
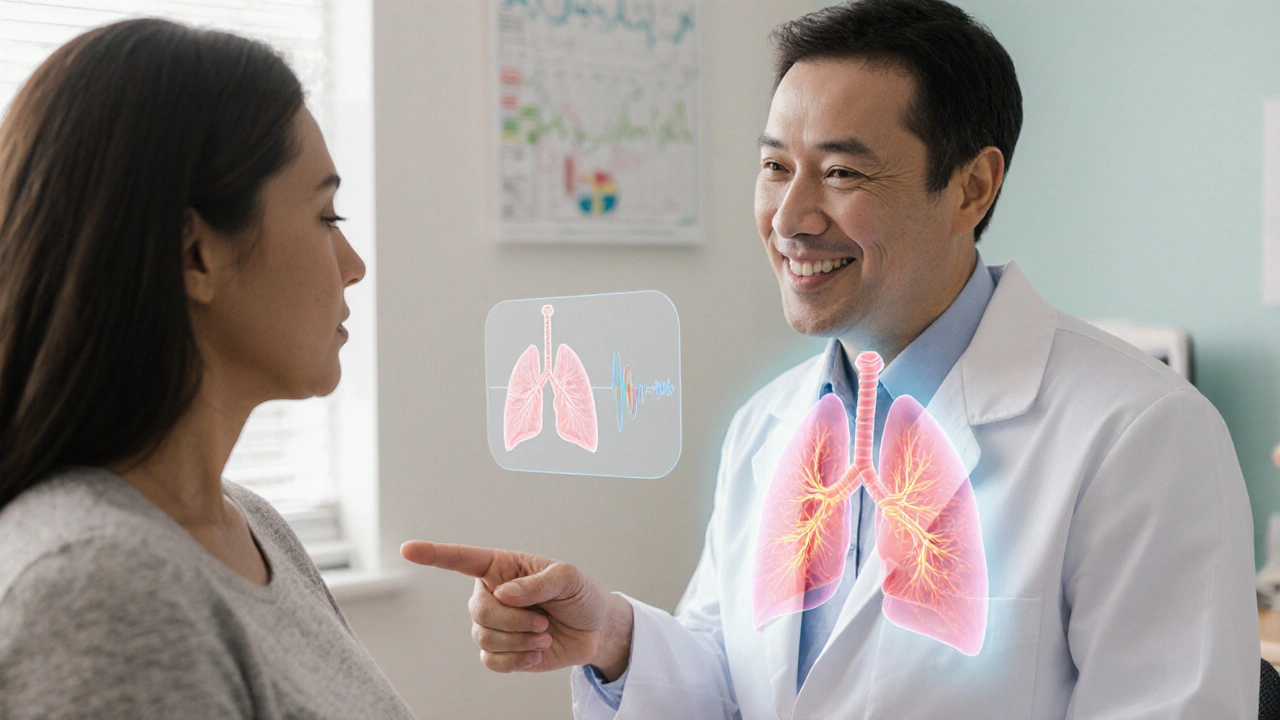
How doctors spot a problem
The first line of defense is the routine check‑up. Primary care physicians often ask simple questions: "Do you wake up short of breath?" or "Do you need an inhaler to run up stairs?" Those answers trigger objective tests.
- Spirometry measures the amount and speed of air you can exhale - the go‑to for asthma and COPD.
- Pulse oximetry checks oxygen saturation in the blood - spotlights hidden hypoxia in sleep apnea and advanced COPD.
- Chest X‑ray or CT scan - visualizes structural changes.
- Allergy testing - identifies triggers that worsen asthma.
When a specialist steps in, a pulmonologist may order a full pulmonary function test battery, or request a home‑based sleep study for suspected apnea.

Treatment kicks in early - why it works better
Once a diagnosis lands, treatment plans can be tailored. Early‑stage asthma often responds to low‑dose inhaled corticosteroids, keeping flare‑ups at bay without heavy medication. For COPD caught before severe obstruction, quitting smoking plus bronchodilator therapy can halt progression.
Sleep apnea is a prime example of the power of early action. If a CPAP (continuous positive airway pressure) machine is introduced before cardiovascular strain builds, patients see a 40% drop in blood pressure within three months. That’s why we stress early diagnosis breathing disorders as a life‑saving move.
- Inhaler therapy delivers medication directly to the lungs - fast relief, fewer systemic side effects.
- CPAP keeps the airway open during sleep - reduces apnea events dramatically.
- Lifestyle tweaks - weight loss, exercise, allergen avoidance.
Real‑world stories that illustrate the difference
Take Maya, a 9‑year‑old from Melbourne who complained of “tight chest” during soccer. Her school nurse suggested a simple peak‑flow test. The result flagged asthma, and a low‑dose inhaler was prescribed. Within weeks, Maya’s performance improved, and she avoided the emergency department visit her brother endured at age 5.
Contrast that with Tom, 58, who ignored a lingering cough for years. By the time a spirometry test revealed moderate COPD, his lungs had already lost 30% of functional capacity. The required medication regimen is now aggressive, and he spends regular nights on oxygen support.
These anecdotes highlight how the same set of symptoms can lead to wildly different outcomes based on timing.
Practical checklist for you or your loved ones
- Schedule a routine health check at least once a year.
- Ask about night‑time breathing patterns - snoring, pauses, gasping.
- Note any exercise‑induced shortness of breath or wheeze.
- If asthma or COPD runs in the family, request spirometry even without symptoms.
- Keep a symptom diary - date, activity, severity - to show doctors.
- Don’t delay a referral to a pulmonologist when tests are abnormal.
- Follow prescribed inhaler technique; misuse reduces effectiveness by up to 50%.
- For suspected sleep apnea, ask about a home sleep test before costly lab studies.
What to do if you’re already diagnosed
Even if you’ve lived with a breathing disorder for years, there’s room to improve. Review your medication list with a pharmacist - many inhalers have newer, lower‑dose options. Ask your doctor about a repeat spirometry; lung function can improve with proper management.
Consider a pulmonary rehab program. These multidisciplinary classes combine breathing exercises, nutrition advice, and strength training, and they’ve been shown to cut hospital admissions by 25% for COPD patients.
Future trends - making early detection even easier
Technology is closing the gap. Portable spirometers now plug into smartphones, giving patients instant feedback. AI‑driven analysis of cough sounds can flag potential asthma or COVID‑related lung issues before a doctor sees you.
Wearable pulse oximeters track oxygen levels throughout the night, alerting users to unexplained drops that could signal sleep apnea. As these tools become affordable, the barrier to early diagnosis shrinks dramatically.
Frequently Asked Questions
How early is too early for a breathing test?
If you notice any recurring shortness of breath, wheeze, or night‑time breathing interruptions, a simple spirometry or pulse oximetry can be done at any age. Pediatric screening is especially valuable for asthma.
Can I self‑diagnose using a home device?
Home devices are great for monitoring trends, but they don’t replace a professional evaluation. Bring your readings to a doctor for interpretation.
What lifestyle changes complement medical treatment?
Quit smoking, maintain a healthy weight, stay active, and reduce exposure to known allergens. These steps boost lung capacity and lower medication needs.
Is CPAP safe for long‑term use?
Yes, when fitted correctly. Regular cleaning and annual mask checks prevent irritation and ensure effectiveness.
How often should I repeat lung function tests?
For stable asthma, once a year is typical. COPD patients may need tests every six months, especially after a flare‑up.










Johnny X-Ray
30 Sep 2025 at 16:20Wow, this tool is a game‑changer! 😊 It really shines a light on hidden breathing issues before they become life‑threatening.