Blood Thinner Complications: Risks, Signs, and How to Stay Safe
When you take a blood thinner, a medication that prevents dangerous blood clots. Also known as anticoagulants, it helps protect against strokes, heart attacks, and pulmonary embolisms—but it also opens the door to serious side effects if not managed carefully. These drugs don’t make your blood "thin" like water. Instead, they slow down your body’s clotting process. That’s helpful when you have atrial fibrillation, a replaced heart valve, or deep vein thrombosis. But when that balance tips too far, even a small bump can lead to dangerous bleeding inside your body.
Not all blood thinners are the same. Warfarin, an older anticoagulant that requires regular blood tests is still used, but many people now take newer options like DOACs, direct oral anticoagulants such as apixaban or rivaroxaban. These don’t need weekly INR checks, but they’re not safer for everyone. If you have kidney problems, your body can’t clear them properly—and that raises your risk of bleeding. Even a slight drop in kidney function can turn a normal dose into a dangerous one. And if you’re over 65, take other meds like NSAIDs or antidepressants, or have a history of stomach ulcers, your risk goes up fast.
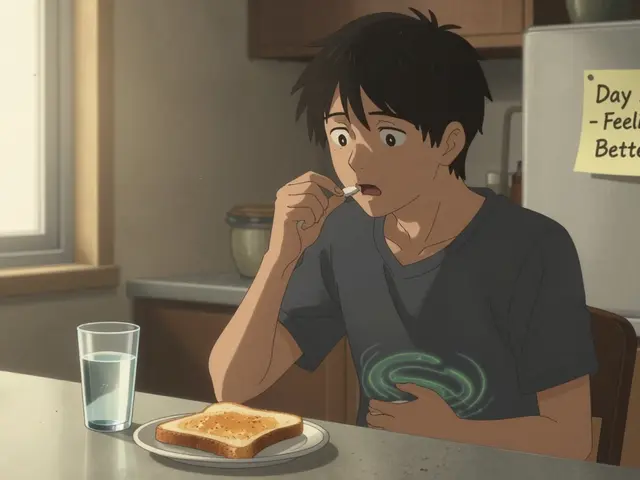
What should you watch for? A nosebleed that won’t stop, gums that bleed when you brush, pink or red urine, black or tarry stools, or a headache that feels worse than any you’ve had before. These aren’t normal. Bruising without injury? That’s a red flag. If you fall hard, even if you feel fine, get checked. Internal bleeding doesn’t always show up right away. Some people don’t realize something’s wrong until they collapse. And here’s the thing: many of these complications happen because patients don’t know how their other meds interact. A common painkiller like naproxen can double your bleeding risk. Grapefruit juice? It messes with how your body handles some of these drugs. Even herbal supplements like garlic, ginkgo, or fish oil can turn a safe dose into a risky one.
You’re not alone in this. Thousands of people manage blood thinners without major issues—but it takes attention, not luck. It’s not about avoiding the medicine. It’s about knowing how to use it right. That means tracking your symptoms, talking to your pharmacist about every new pill or supplement, and never skipping a follow-up. The posts below cover real cases: how kidney disease changes DOAC dosing, why hypothyroidism makes muscle damage worse when you’re on statins, how to spot early signs of internal bleeding, and what to do when a medication you’ve taken for years suddenly becomes risky. You’ll find practical advice from people who’ve been there—not theory, not guesswork. This isn’t about fear. It’s about control.
Heparin-induced thrombocytopenia (HIT) is a rare but life-threatening reaction to heparin that causes low platelets and dangerous blood clots. Learn the symptoms, risk factors, and how it’s diagnosed and treated.