When your kidneys aren’t working right, what you eat matters more than you might think. Especially protein. Too much can overload your kidneys. Too little can leave you weak, tired, and at risk for muscle loss. The trick isn’t just cutting back-it’s getting the right amount of the right kind of protein for your stage of chronic kidney disease (CKD). And it’s not one-size-fits-all.
What Protein Does (and Doesn’t Do) for Your Kidneys
Your kidneys filter waste from your blood. When you eat protein, your body breaks it down into nitrogen-based waste like urea. Healthy kidneys handle this easily. But when kidney function drops, that waste builds up. That’s why protein restriction has been used for over 100 years to ease the burden.
But here’s the catch: protein isn’t just about waste. It’s also about survival. Muscle loss, fatigue, and poor healing are common in later stages of CKD. Studies show that 30-50% of people with stage 3-5 CKD develop protein-energy wasting. That’s not just being thin-it’s losing muscle mass, which raises your risk of infection, hospitalization, and death.
So the goal isn’t to starve yourself of protein. It’s to find the sweet spot: enough to keep your body strong, but not so much that your kidneys are overwhelmed.
Protein Targets by CKD Stage
Not all CKD is the same. Your protein needs change as your kidneys decline. Here’s what the latest guidelines say, broken down by stage.
CKD Stage 1-2 (GFR ≥60 mL/min): Your kidneys are still working fairly well, but damage is present. The Kidney Health Initiative recommends no more than 0.8 grams of protein per kilogram of your ideal body weight. For a 150-pound person (68 kg), that’s about 54 grams a day. Some newer research, like the 2024 JAMA Network Open study, suggests that for older adults, slightly higher intake-up to 1.0-1.3 g/kg-may actually lower death risk, even if it doesn’t slow kidney decline. The key? If you’re over 65 and not losing weight, don’t panic if you’re eating a bit more.
CKD Stage 3 (GFR 30-59 mL/min): This is where things get more precise. The KDOQI guidelines suggest 0.55-0.60 g/kg/day. For our 150-pound person, that’s 40-54 grams daily. Many people find this range hard to hit without help. You’re not supposed to drop to 20 grams. That’s dangerous. You’re aiming for balance.
CKD Stage 4 (GFR 15-29 mL/min): Protein needs tighten further. DaVita recommends 0.6 g/kg, with half of it coming from high-quality sources. That means eggs, milk, chicken, fish, lean beef, and soy. These provide all the essential amino acids your body can’t make on its own. If you’re diabetic, the American Diabetes Association suggests 0.8-0.9 g/kg to protect your muscles without spiking blood sugar.
CKD Stage 5 (GFR <15 mL/min, not on dialysis): This is the most delicate stage. Protein intake drops to 0.55-0.60 g/kg, but only if you’re not losing weight. If you’re already underweight or losing muscle, your doctor might raise the target. Many patients here use keto acid analogues like Ketosteril-supplements that help your body make protein without creating extra waste. These are prescribed in about 15% of European stage 4-5 cases.
Plant vs. Animal Protein: The Real Difference
Not all protein is created equal-especially for your kidneys.
Animal proteins (meat, dairy, eggs) are called “high-quality” because they contain all nine essential amino acids. But they also produce 20-30% more urea and phosphate than plant proteins. They also generate more advanced glycation end products (AGEs), which cause inflammation and oxidative stress in damaged kidneys.
Plant proteins (beans, lentils, tofu, nuts, quinoa) are gentler on the kidneys. A 2021 meta-analysis found that replacing just 30% of animal protein with plant protein lowered CKD progression risk by 14% and cut death risk by 11%. Sounds great, right?
But here’s the problem: most plant proteins are low in lysine and methionine. If you eat only beans and rice, you might not get enough complete protein. That’s why experts recommend combining sources-like beans with rice, or hummus with whole grain pita. Soy is the exception. It’s a complete plant protein and works well in CKD diets.
And there’s another catch: plants are high in potassium. For stage 4-5 patients who need to limit potassium, that’s a problem. A baked potato might be healthy for someone without kidney disease-but dangerous for someone with stage 5 CKD. So while plant-based diets help, they require careful planning.
Why So Many People Struggle
It’s not just about knowing the numbers. It’s about living them.
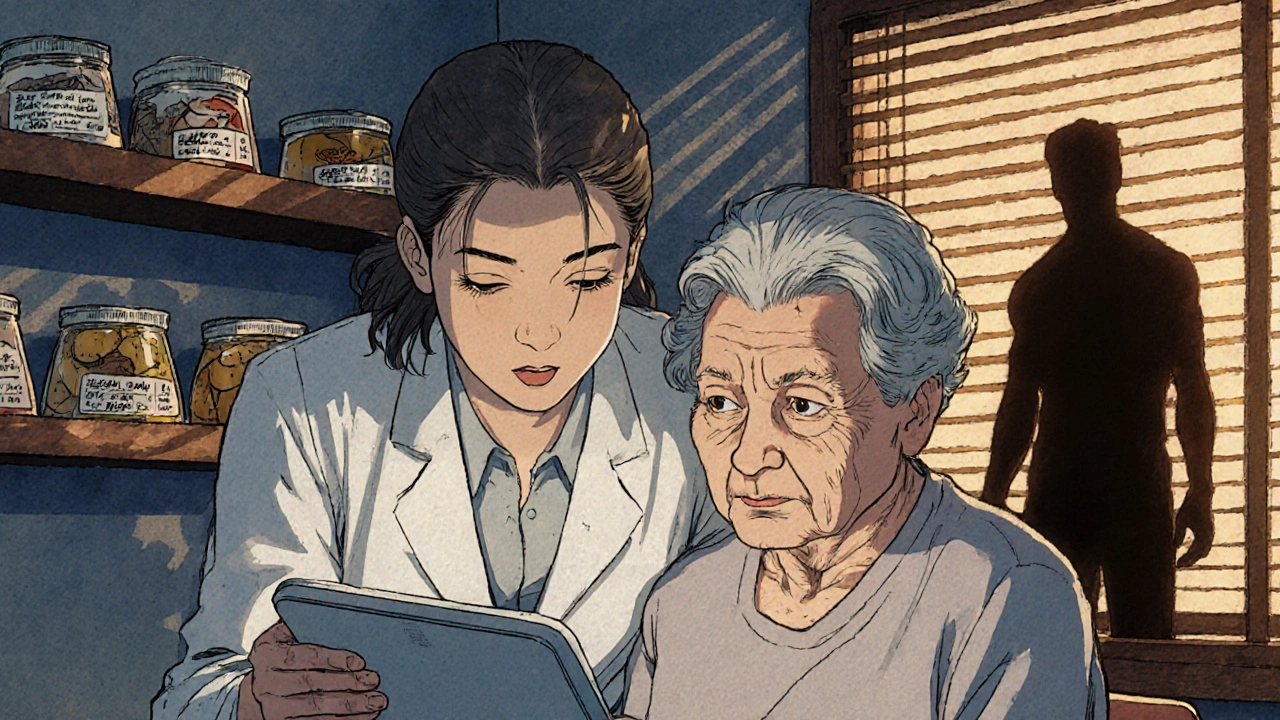
On patient forums, 74% of people say they feel constantly hungry after cutting protein. 62% report muscle weakness. 58% say they avoid social meals because they can’t eat what everyone else is having. One Reddit user wrote: “Cutting my protein from 100g to 45g made me feel like I was dying slowly.”
That’s why working with a renal dietitian makes such a difference. DaVita’s survey found that 82% of patients who got personalized meal plans reported better energy, less hunger, and improved quality of life. Those who didn’t? Only 24% stuck with the plan.
Common roadblocks:
- Tracking protein in mixed dishes (like casseroles or stir-fries)-87% of patients struggle with this.
- Juggling protein, potassium, and phosphorus at the same time-76% say it’s overwhelming.
- Getting enough calories without too much protein-63% report unintentional weight loss.
Solutions that work:
- Using apps like MyFitnessPal with renal-specific food databases (used by 42% of patients).
- Meal prepping with renal-friendly recipes from Kidney Kitchen (visited 1.2 million times a month).
- Using the NKF’s free Protein Target Calculator app (downloaded over 47,000 times since 2023).
What Experts Really Think
There’s debate-and it’s real.
Dr. T. Alp Ikizler, who helped write the KDOQI guidelines, says: “The evidence for protein restriction in stages 3b-5 is strong. We’ve seen a 32% lower risk of needing dialysis when people stick to 0.6-0.8 g/kg.”
But Dr. Kamyar Kalantar-Zadeh, a leading nephrologist, counters: “For older adults, the bigger threat isn’t kidney failure-it’s heart disease. Many die before they ever reach dialysis. If cutting protein makes you weak and malnourished, you’re trading one risk for a deadlier one.”
The National Kidney Foundation’s 2023 consensus says it best: individualize. Your age, weight, muscle mass, diabetes status, and how you’re feeling matter more than any chart.
The 2022 Cochrane Review found low-protein diets reduced ESRD risk by 31%-but only 58% of patients could stick to them. That’s the real problem. A perfect diet that you can’t live with isn’t a solution.
How to Get Started
You don’t need to figure this out alone. Here’s how to begin:
- Ask your nephrologist for a referral to a renal dietitian. Medicare now covers 3 hours of initial nutrition counseling and 2 hours of follow-up per year for CKD patients.
- Calculate your ideal body weight. Use online tools or ask your dietitian. Don’t use your current weight if you’re overweight or underweight.
- Start tracking your protein intake for a week. Use an app or a food diary. You’ll be shocked how quickly protein adds up.
- Focus on quality. Prioritize eggs, fish, chicken, and soy. Limit red meat and processed meats.
- Combine plant proteins. Eat beans with rice, lentils with whole wheat bread. Don’t rely on one source.
- Check your calories. If you’re losing weight, you’re not eating enough-even if you’re eating “the right” protein.
It takes 3-6 months to feel comfortable with this diet. Don’t expect perfection right away. Small changes-like swapping a beef burger for a tofu stir-fry-add up over time.
The Future of Renal Nutrition
The next wave isn’t just about grams per kilogram. It’s about personalization.
The NIH-funded PRECISE-CKD trial is testing whether protein targets should be based on your individual urea production-not just your weight. Some people naturally make more waste than others. Why treat everyone the same?
Companies are also developing plant-based protein concentrates with reduced potassium. Imagine a soy protein powder that doesn’t spike your potassium levels. That could be a game-changer.
And machine learning? It’s being used to predict who will benefit most from protein restriction based on genetics, blood markers, and eating habits. This isn’t sci-fi-it’s happening now.
But here’s the bottom line: 92% of nephrologists agree that protein management will stay central to CKD care through 2030. The shift? Less focus on strict limits. More focus on quality, balance, and individual needs.
Your kidneys are telling you something. Listen-not by starving yourself, but by eating smarter.
How much protein should I eat if I have CKD stage 3?
For CKD stage 3, aim for 0.55 to 0.60 grams of protein per kilogram of your ideal body weight each day. For a person weighing 150 pounds (68 kg), that’s about 40 to 54 grams daily. This range helps slow kidney damage without causing muscle loss. Always confirm your target with a renal dietitian, especially if you’re diabetic or losing weight.
Can I eat plant-based protein with CKD?
Yes, and it’s often better for your kidneys. Plant proteins produce less waste and reduce inflammation. But they’re lower in essential amino acids like lysine and methionine. Combine sources-like beans with rice or hummus with whole grain bread-to get complete protein. Watch potassium levels, especially in stage 4-5, and avoid high-potassium plants like spinach, potatoes, and bananas unless they’re soaked or boiled.
Why do I feel weak on a low-protein diet?
You might not be eating enough total calories or high-quality protein. Feeling weak is a sign of muscle loss, which is common in later CKD stages. Make sure half your protein comes from eggs, fish, chicken, or soy. Add healthy fats like olive oil and avocado to boost calories without adding protein. Talk to a dietitian-you may need supplements or keto acid analogues.
Is it safe to eat more protein if I’m older with CKD?
For older adults (over 65), higher protein intake-up to 0.8-1.0 g/kg-may be safer than strict restriction. Many die from heart disease before reaching dialysis, and muscle loss increases fall risk and infection. Studies show older CKD patients on higher protein diets live longer. But this only applies if you’re not losing weight and have no severe fluid retention. Always check with your doctor.
Do I need to take protein supplements for CKD?
Most people don’t. Real food is better. But if you’re struggling to meet your protein goal without exceeding phosphorus or potassium, your doctor might prescribe keto acid analogues like Ketosteril. These supplements help your body build protein without creating waste. They’re not over-the-counter-they require a prescription and are usually used in stage 4-5 CKD. Don’t buy regular protein powders; most are too high in phosphorus and potassium.
How do I track protein in meals like soup or pasta?
Use apps like MyFitnessPal with renal-specific food databases, or ask your dietitian for a list of common portion sizes. For example, 1 cup of cooked pasta has about 7g protein, 3 oz of chicken has 21g, and 1/2 cup of beans has 7g. Weigh your food at first. Over time, you’ll learn to estimate. Avoid guessing-87% of patients misjudge protein in mixed dishes.








Chris Taylor
30 Nov 2025 at 11:10I used to think cutting protein meant eating salad forever. Turns out, I was just starving myself and feeling like a zombie. Found a renal dietitian and now I eat eggs, chicken, and even some cheese without guilt. My energy is back, and my labs are stable. It’s not about restriction-it’s about smart choices.