Heart Failure Fluid Retention Calculator
Understand Your Risk
NSAIDs like ibuprofen and naproxen can cause dangerous fluid retention in heart failure patients. This calculator estimates your potential fluid retention and risk level based on how you take these medications.
Calculate Your Fluid Retention Risk
Results will appear here after calculation
Many people reach for ibuprofen or naproxen when they have a headache, sore knee, or back pain. It’s quick, cheap, and available over the counter. But if you have heart failure, taking these common painkillers could land you in the hospital - sometimes within just a few days.
Why NSAIDs Are Dangerous for Heart Failure Patients
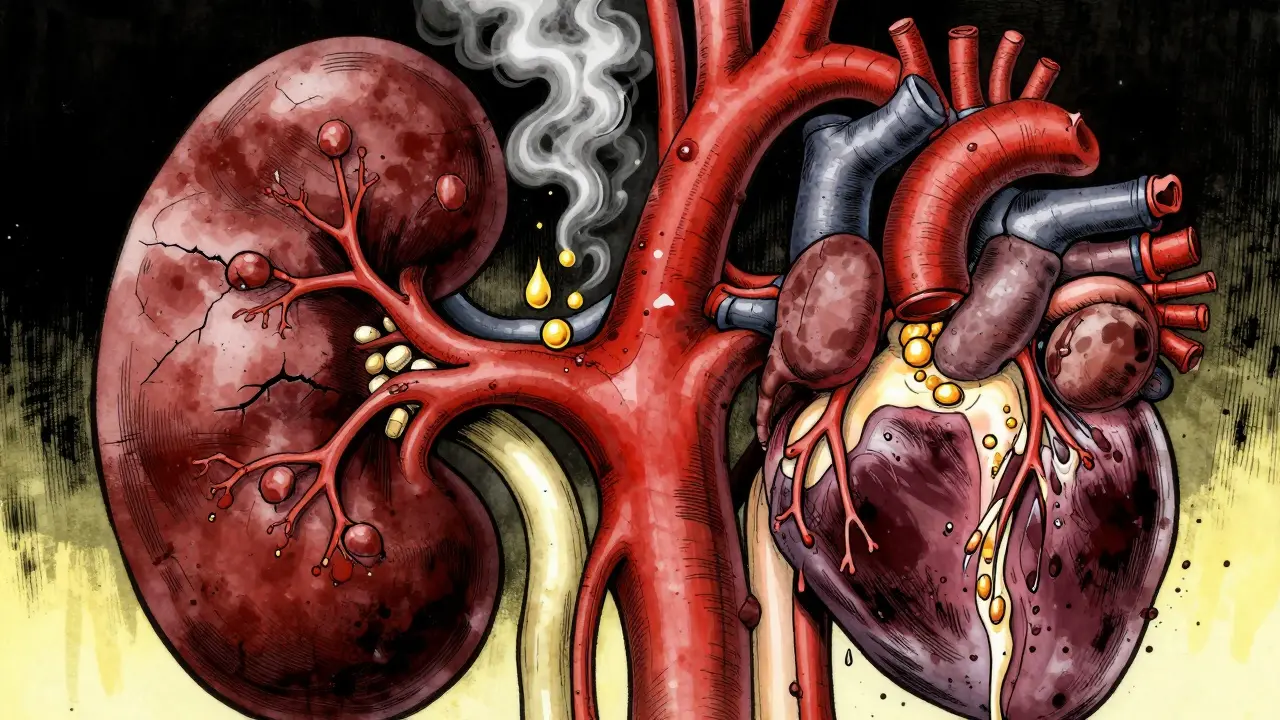
NSAIDs - non-steroidal anti-inflammatory drugs - work by blocking enzymes called COX-1 and COX-2. These enzymes help make prostaglandins, chemicals that cause pain and swelling. But prostaglandins also play a key role in keeping your kidneys working properly. When NSAIDs block them, your kidneys start holding onto sodium and water. That extra fluid doesn’t just sit in your ankles. It floods your bloodstream, increasing the workload on your heart.For someone with heart failure, that’s like adding weight to a struggling engine. The heart is already weak. It can’t pump efficiently. Now it has to move more blood, faster, against higher pressure. The result? Fluid backs up into the lungs, legs, and abdomen. Symptoms like swelling, sudden weight gain, and shortness of breath appear quickly - sometimes within 24 to 72 hours.
A 2022 study in the European Heart Journal followed over 100,000 people in Denmark with type 2 diabetes, a group already at high risk for heart failure. The researchers found that even a few days of NSAID use - including ibuprofen, naproxen, and celecoxib - raised the chance of hospitalization for heart failure by up to 88%. The highest risk? The first week after starting the drug.
It’s Not Just Prescription NSAIDs
A lot of people think the danger only comes from strong, prescription-strength NSAIDs. That’s not true. Over-the-counter pills like Advil, Motrin, and Aleve carry the same risks. In fact, the problem is worse because people don’t realize they’re taking something dangerous.A 2018 survey by the American Heart Association found that 37% of heart failure patients had taken NSAIDs without knowing they were at risk. Of those, 62% ended up with worsening symptoms that needed emergency care. One Reddit user shared how he took two 400mg doses of ibuprofen for a bad back. Within three days, he gained 4.5 kilograms (10 pounds) of fluid. He ended up in the hospital with acute heart failure.
Even topical NSAIDs - gels and patches - aren’t safe. While they seem less harmful because they’re applied to the skin, studies show enough of the drug still gets into your bloodstream to affect your kidneys and heart.
COX-2 Inhibitors Are Not Safer
For years, doctors thought drugs like celecoxib (Celebrex) were safer because they didn’t irritate the stomach as much. But when it came to the heart and kidneys, they turned out to be just as dangerous.A 2003 review by Dr. Gysèle Bleumink showed that COX-2 inhibitors like celecoxib reduce kidney blood flow and cause fluid retention just like older NSAIDs. This was confirmed again in 2019 by New Zealand’s Medsafe agency, which updated its warning to say: “All NSAIDs, including COX-2 selective inhibitors, can worsen heart failure.”
There’s no magic bullet here. No NSAID is truly safe for someone with heart failure. Even naproxen, sometimes called the “least risky” NSAID, still carries a measurable increase in hospitalization risk. The European Society of Cardiology’s 2021 guidelines give NSAIDs a Class III recommendation - meaning they’re proven to cause harm and should be avoided entirely.
Who’s Most at Risk?
Not everyone with heart failure will react the same way. But some groups are far more vulnerable:- People over 65 - kidneys naturally decline with age, making them more sensitive to NSAID effects
- Those with type 2 diabetes - diabetes already damages kidney function
- People with reduced ejection fraction - their hearts are weaker and less able to handle extra fluid
- Anyone on diuretics or ACE inhibitors - NSAIDs interfere with how these heart medications work
One study found that 22.3% of heart failure patients with preserved ejection fraction still got NSAID prescriptions within a year of diagnosis. That’s alarming. These patients often feel better and assume they’re “not that sick.” But their hearts are still struggling. Even a small fluid overload can tip them into crisis.
What Happens in the Body?
Here’s the science behind the symptoms:- NSAIDs block prostaglandins in the kidneys
- Without prostaglandins, the kidneys reabsorb more sodium and water
- Extra sodium pulls in more fluid, increasing blood volume
- The heart has to pump harder to move the extra blood
- Fluid leaks into tissues - causing swelling in legs, ankles, and lungs
- Shortness of breath, fatigue, and rapid weight gain follow
This isn’t a slow, gradual process. It can happen fast. A 2024 study in the Global Heart Failure Registry showed that patients exposed to NSAIDs within 30 days of leaving the hospital had a 28% higher chance of being readmitted - and often within just 7 days.

What Can You Take Instead?
Acetaminophen (Tylenol) is the go-to alternative. It doesn’t affect kidney blood flow or sodium balance the way NSAIDs do. It won’t reduce inflammation like ibuprofen, but it’s safe for pain and fever in heart failure patients.For chronic joint pain, non-drug options are better: physical therapy, heat/cold packs, weight management, and low-impact exercise like swimming or walking. Some patients find relief with topical capsaicin cream or transcutaneous electrical nerve stimulation (TENS) units.
Never assume a “natural” remedy is safe. Herbal supplements like willow bark or turmeric can have aspirin-like effects and carry similar risks. Always check with your doctor or pharmacist before trying anything new.
What Should Doctors and Caregivers Do?
Doctors need to ask about NSAID use - not just prescription meds, but everything the patient takes. A 2021 survey found that only 43% of primary care doctors routinely check for NSAID use during medication reviews.Family members can help. If someone with heart failure says they’re taking Advil for their arthritis, speak up. Keep a list of all medications and supplements. Watch for sudden weight gain (more than 2 kg in 2 days), swollen ankles, or trouble breathing at night.
Some hospitals now use digital alerts in electronic records to flag NSAID prescriptions for heart failure patients. The American College of Cardiology is developing a mobile app for heart failure patients that will send alerts if someone tries to order ibuprofen online or scans a pharmacy barcode. It’s set to launch in mid-2025.
The Bottom Line
NSAIDs are not harmless pain relievers for people with heart failure. They are a hidden danger - one that can turn a stable condition into a medical emergency in less than a week. There’s no safe dose, no safe duration, and no safe type.If you have heart failure, avoid all NSAIDs. Not just the strong ones. Not just the prescription ones. All of them.
Use acetaminophen for pain. Talk to your doctor about non-drug options. And if you’ve already taken an NSAID and feel worse - swollen, breathless, or gaining weight fast - call your doctor immediately. Don’t wait. This isn’t something you can tough out. It’s a sign your heart is under stress - and it needs help now.









Lynsey Tyson
18 Dec 2025 at 16:36I had no idea ibuprofen could do this. My grandma’s on heart meds and she swears by her Advil for her knees. I’m gonna have a serious talk with her tonight. Thanks for the wake-up call.
Just saved her from a hospital trip.