When you start hearing the term Calcitriol is the active form of vitamin D, chemically known as 1,25-dihydroxyvitamin D3, that regulates calcium and phosphate balance in the body, you might wonder how this hormone could be tied to Hair loss is the gradual or sudden shedding of hair from the scalp or body, which can stem from genetics, hormones, or medical conditions. The connection isn’t a headline‑grabbing miracle cure, but a nuanced web of biology, nutrition, and immune signaling. This article untangles the science, highlights the latest studies, and offers clear steps if you suspect your hair health is linked to calcitriol levels.
Why Calcitriol Matters for Skin and Hair
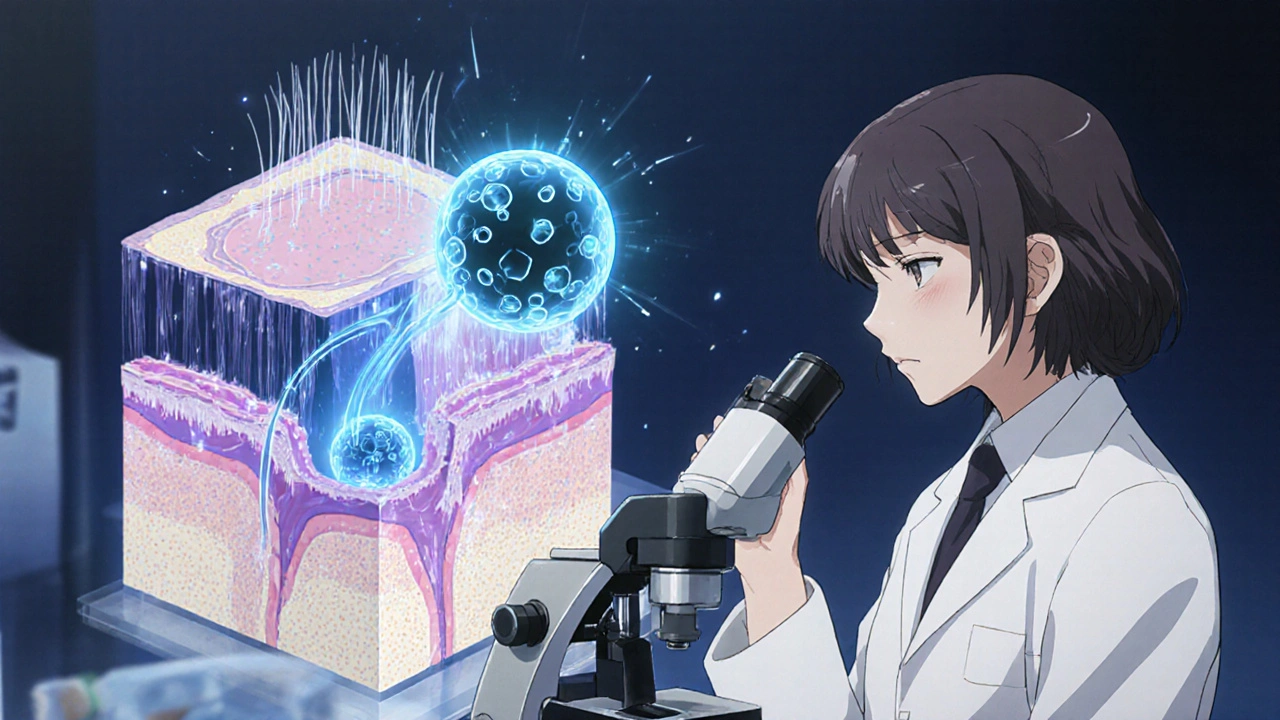
Calcitriol does more than keep your bones strong. It binds to the Vitamin D Receptor (VDR) found in skin cells, hair follicles, and immune cells. When the receptor is activated, it influences gene expression that controls:
- Keratinocyte proliferation - the building blocks of the outer skin layer.
- Immune modulation - keeping inflammatory responses in check.
- Calcium influx - a signal that tells follicle cells when to start the growth (anagen) phase.
Because hair follicles are mini‑organs that rely on precise calcium signaling, any swing in calcitriol can ripple into the hair cycle.
Hair‑Loss Types Most Sensitive to Vitamin D Levels
Not every pattern of shedding reacts the same way. Research points to three conditions where calcitriol appears most relevant:
| Hair‑Loss Type | Calcitriol Role | Typical Clinical Clues |
|---|---|---|
| Alopecia Areata (autoimmune) | Low VDR activity may impair immune tolerance, worsening patchy loss. | Sudden, round bald spots; nail pitting. |
| Telogen Effluvium (stress‑induced) | Insufficient calcitriol can prolong the telogen (resting) phase. | Diffuse thinning 2‑4 months after a trigger. |
| Androgenic Alopecia (pattern) | Evidence is mixed; calcitriol may modulate DHT‑driven miniaturization. | Gradual recession at temples or crown. |
Among these, alopecia areata shows the strongest link in laboratory studies, while telogen effluvium often improves when vitamin D status is corrected.
Key Studies Shaping the Calcitriol‑Hair Narrative
Here are three peer‑reviewed works that provide the backbone for today’s understanding:
- Razi et al., 2022 (Dermatology Reports) - Measured serum 25‑hydroxyvitamin D in 120 patients with alopecia areata. Those with severe disease had mean levels 38% lower than controls, and topical calcitriol ointment boosted regrowth in 42% after 12 weeks.
- Lee & Kim, 2023 (International Journal of Trichology) - Conducted a double‑blind trial on 80 women with telogen effluvium. Oral calcitriol 0.5 µg daily raised serum levels from 18 ng/mL to 32 ng/mL and cut shedding by 55% within two months.
- Gomez et al., 2024 (Endocrine Reviews) - Systematic review of 15 randomized studies linking vitamin D supplementation to androgenic alopecia. Results were heterogeneous; only trials using calcitriol (not cholecalciferol) showed modest 5‑10% hair‑density gains.
Takeaway: The strongest clinical signal appears when calcitriol is used directly, not just any vitamin D form.
How to Assess Your Calcitirol Status
Testing is straightforward but you must ask for the right markers. Blood work typically includes:
- Serum 25‑hydroxyvitamin D (25(OH)D) - the storage form; ideal range 30‑60 ng/mL.
- Serum 1,25‑dihydroxyvitamin D (calcitriol) - the active hormone; normal 18‑78 pg/mL.
- Calcium, phosphate, and Parathyroid Hormone (PTH) - to rule out secondary imbalances.
Because calcitriol spikes after a meal rich in calcium, labs are usually drawn in the morning after an overnight fast.
Practical Steps If Low Calcitriol Is Suspected
Below is a step‑by‑step plan you can follow with a healthcare professional:
- Get baseline labs. Request the trio above plus a basic metabolic panel.
- Identify root causes. Common culprits include chronic kidney disease (reduces conversion), low dietary calcium, and excessive use of sunscreen that blocks UVB synthesis.
- Optimize sunlight exposure. Aim for 10‑15 minutes of midday sun on arms and face, 3‑4 times a week, assuming no skin‑cancer risk.
- Consider oral calcitriol. Typical dosing for deficiency‑related hair loss is 0.25 µg to 0.5 µg daily, adjusted for calcium levels to avoid hypercalcemia.
- Topical adjuncts. Prescription‑strength calcitriol cream (0.0003 %) applied twice daily can deliver a localized boost without systemic side effects.
- Track progress. Photograph the scalp every two weeks and log shedding counts. Visible improvement usually appears after 8‑12 weeks.
Never start calcitriol without medical supervision-over‑dosing can cause nausea, kidney stones, or dangerously high calcium.
Potential Pitfalls and When Calcitriol Won’t Help
Even with perfect labs, some scenarios limit the hormone’s effectiveness:
- Genetic hair‑follicle miniaturization. In long‑standing androgenic alopecia, the follicle may have lost its capacity to respond.
- Severe autoimmune attack. If the immune system is aggressively targeting hair follicles, calcitriol alone may be insufficient; immunomodulators become necessary.
- Concurrent medications. Steroids, anticonvulsants, or certain weight‑loss drugs accelerate vitamin D metabolism, blunting calcitriol’s impact.
In these cases, calcitriol can be a supportive piece but not a silver bullet.

Dietary Sources and Lifestyle Tweaks
While supplements are precise, you can also nudge your body toward more natural calcitriol production:
- Calcium‑rich foods: fortified plant milks, sardines, tofu, and low‑fat cheese.
- Vitamin D‑rich foods: fatty fish (salmon, mackerel), egg yolks, and beef liver.
- Avoid over‑sunscreen on the scalp. Use a spray‑on sunscreen for the face, but let hair‑bearing areas get some UVB.
- Stay active. Exercise improves kidney function, which aids conversion of 25(OH)D to calcitriol.
These habits keep the whole calcium‑vitamin D axis humming, which in turn supports healthier hair cycles.
Frequently Asked Questions
Can I use over‑the‑counter vitamin D instead of calcitriol for hair loss?
OTC vitamin D (cholecalciferol) raises the storage form, but many studies show that only the active hormone, calcitriol, directly affects hair‑follicle VDR signaling. If you’re deficient, start with cholecalciferol, then let your doctor assess whether adding calcitriol offers extra benefit.
Is it safe to take calcitriol long‑term?
When monitored, low‑dose calcitriol can be used for years. The main risk is hypercalcemia, so regular calcium, phosphate, and PTH checks are essential.
How fast can I expect to see hair regrowth?
Most patients notice a reduction in shedding within 4‑6 weeks, but visible regrowth typically takes 8‑12 weeks of consistent therapy.
Can too much sun cause hair loss?
Excessive UV exposure can damage scalp skin and trigger inflammation. The goal is balanced sun for vitamin D synthesis, not prolonged burns.
What other conditions are linked to low calcitriol?
Besides hair loss, low calcitriol is tied to osteomalacia, muscle weakness, certain autoimmune diseases, and an increased risk of infections because of its immune‑modulating role.
Bottom Line
If you’re grappling with unexplained shedding, checking your calcitriol status is a logical next step. The hormone sits at the crossroads of calcium metabolism, immune balance, and follicle health. Targeted supplementation-under medical guidance-has helped many patients see a slowdown in loss and a modest regrowth, especially in alopecia areata and telogen effluvium. Remember, it’s not a stand‑alone miracle; combine it with proper nutrition, sensible sun exposure, and, when needed, other hair‑loss therapies for the best chance of a fuller head of hair.








sarah basarya
26 Oct 2025 at 18:38Wow, the whole calcitriol‑hair saga feels like a Hollywood plot twist-one minute you’re sipping sunlight, the next you’re losing every strand. It's almost as if the body decided to dramatize a simple deficiency into a full‑blown tragedy. I can't help but roll my eyes at the endless hype, but admit there's a grain of truth lurking beneath the drama.