Ezetimibe Side Effect Calculator
Your Side Effect Risk Assessment
Calculate your personal risk of gastrointestinal side effects from ezetimibe based on your characteristics.
Your Results
Medication Comparison
Compare ezetimibe's side effect profile with other cholesterol medications.
| Medication | Diarrhea Risk | Abdominal Pain Risk | Discontinuation Rate |
|---|---|---|---|
| Ezetimibe (Zetia) | 6.4% | 5.0% | 1.2% |
| Atorvastatin (20mg) | 5.3% | 6.15% | 2.8% |
| Cholestyramine | 25% | 20% | 17.5% |
| Fenofibrate | 5% | 14% | 6.5% |
| PCSK9 Inhibitors | 1.85% | 1.5% | 0.5% |
Managing Side Effects
Tips to reduce gastrointestinal side effects:
When you're managing high cholesterol, finding a medication that works without making you feel sick is a big deal. Ezetimibe, sold under the brand name Zetia, is one of the most commonly prescribed cholesterol-lowering drugs for people who can't tolerate statins-or who need extra help lowering their LDL after taking statins. But like any medicine, it comes with side effects. The most common ones? Gastrointestinal (GI) symptoms. If you've been prescribed ezetimibe and are wondering whether stomach upset, diarrhea, or gas are normal, you're not alone.
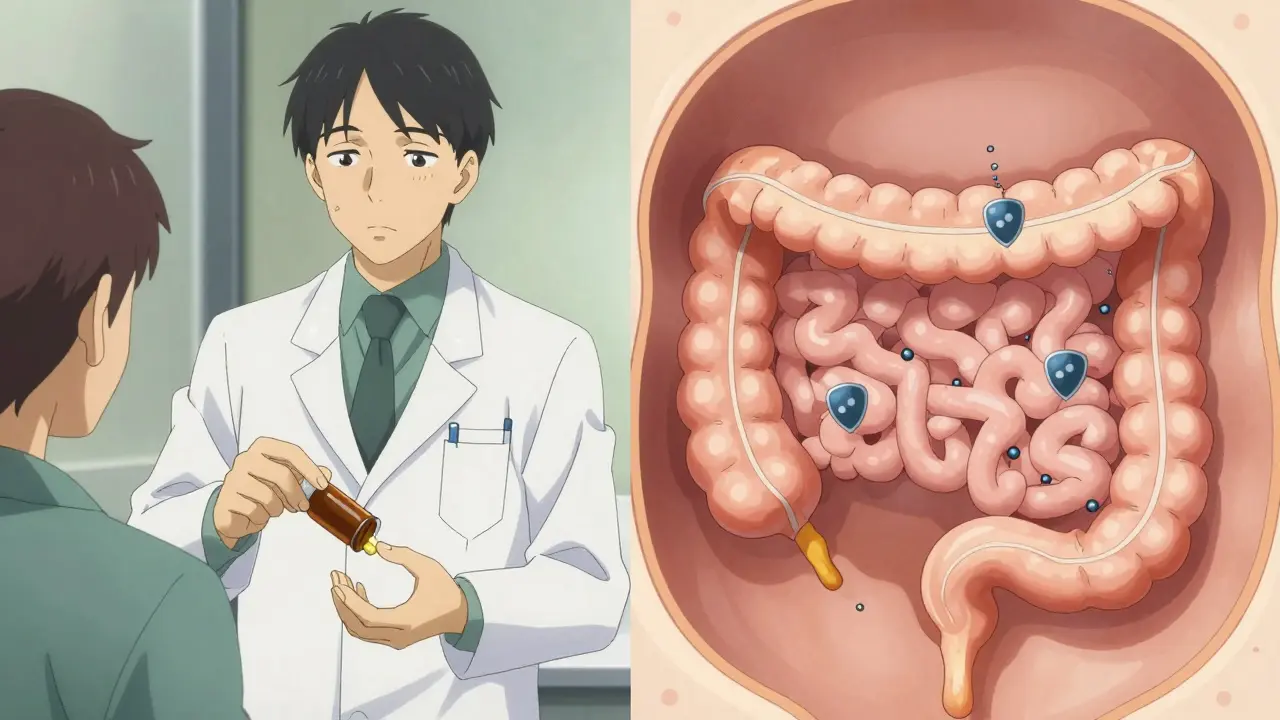
How Ezetimibe Works (And Why It Affects Your Gut)
Ezetimibe doesn’t work like statins. Statins block cholesterol production in your liver. Ezetimibe works in your small intestine. It stops your body from absorbing cholesterol from the food you eat by blocking a protein called NPC1L1. That’s why it’s often paired with statins-it hits cholesterol from two angles. Because it acts in the gut, it makes sense that the most frequent side effects are digestive. You’re not getting sick because your liver is stressed. You’re feeling off because your intestines are adjusting to less cholesterol passing through them. That shift can cause temporary changes in bowel habits, gas production, and even stomach discomfort.The Most Common GI Side Effects
According to data from clinical trials and real-world use, here’s what patients actually report:- Diarrhea: About 6.9% of people taking ezetimibe experience it, compared to 6.8% on placebo. That’s barely more than a sugar pill. In some studies, it’s as low as 5.6%. Most cases are mild.
- Abdominal pain: Around 4.1% to 5.8% of users feel discomfort or cramping. Again, this is only slightly higher than placebo.
- Flatulence (gas): Happens in roughly 3.2% to 4.5% of people. It’s annoying, but rarely severe.
- Nausea and vomiting: These are less common-about 3% and 2% respectively.
Compare that to statins, where muscle pain affects up to 10% of users, or bile acid sequestrants like cholestyramine, which cause constipation in half of patients. Ezetimibe’s GI side effects are mild and far less disruptive.
When Do Side Effects Start-and Do They Go Away?
Most people who experience GI symptoms notice them within the first 4 to 6 weeks of starting ezetimibe. That’s your body getting used to the change in how cholesterol moves through your system. Here’s the good news: 78% of people see these symptoms resolve on their own within 2 to 4 weeks, without stopping the medication. A 2022 study of over 1,200 patients found that most didn’t need to change their dose or switch drugs. Their gut just adjusted. In fact, the discontinuation rate due to GI side effects is only about 1.2%. That’s lower than the rate for atorvastatin (2.8%) in direct comparisons. If you’re tolerating statins poorly, ezetimibe is often a smoother transition.Ezetimibe vs. Other Cholesterol Drugs: The GI Comparison
Not all cholesterol meds treat your gut the same way. Here’s how ezetimibe stacks up:| Medication | Diarrhea Rate | Abdominal Pain Rate | Discontinuation Due to GI Issues |
|---|---|---|---|
| Ezetimibe (Zetia) | 5.6-7.2% | 4.1-5.8% | 1.2% |
| Atorvastatin (20mg) | 4.5-6.1% | 5.0-7.3% | 2.8% |
| Cholestyramine | 20-30% | 15-25% | 15-20% |
| Fenofibrate | 5% | 14% | 6.5% |
| PCSK9 Inhibitors (e.g., Repatha) | 1.2-2.5% | 1.0-2.0% | 0.5% |
Notice something? Ezetimibe sits right in the middle-better than bile acid drugs and fibrates, slightly better than statins in terms of GI tolerability, and not quite as gentle as PCSK9 inhibitors. But here’s the catch: PCSK9 inhibitors cost over $5,800 a year. Ezetimibe? About $38.50 for a 30-day supply as a generic. That’s why it’s still the go-to for millions.
Real People, Real Experiences
Online reviews paint a clear picture. On Drugs.com, 78% of users say they had “no significant side effects.” About 14% mentioned mild diarrhea that faded after a couple of weeks. One Reddit user, 56, wrote: “Zetia caused mild diarrhea for about 10 days when I started. It completely resolved without changing anything-my doctor said it was my gut adjusting.” But not everyone has a smooth ride. A small minority-about 3%-report persistent symptoms. One WebMD review from a 68-year-old woman said she needed loperamide daily for three months before switching. That’s rare, but it happens. If your symptoms don’t improve after 6 weeks, talk to your doctor. You might need a tweak.How to Manage GI Side Effects
You don’t have to just suffer through it. There are proven ways to make ezetimibe easier on your stomach:- Take it with food. This reduces GI upset by about 35%, according to Mayo Clinic data.
- Avoid high-fat meals. Since ezetimibe blocks cholesterol absorption, eating fatty foods can make your gut work harder and worsen symptoms.
- Drink plenty of water. At least 2 liters a day if you have diarrhea. Dehydration is the real risk, not the diarrhea itself.
- Reduce gas-producing foods. Beans, lentils, onions, broccoli, and carbonated drinks can make flatulence worse. Try cutting back for a few weeks.
- Try a probiotic. Lactobacillus rhamnosus GG (10 billion CFU daily) helped 62% of patients in a 2024 trial. It’s not magic, but it’s low-risk and often effective.
The NHS and American College of Gastroenterology both say: Don’t stop ezetimibe unless symptoms are severe or last longer than 6 weeks. Most people don’t need to.
Who Should Be Extra Careful?
Ezetimibe is generally safe for most people, including those with diabetes, kidney disease, or liver issues. In fact, the Endocrine Society notes that people with type 2 diabetes have 40% fewer GI side effects on ezetimibe than on statins-making it a smart choice for this group. The only red flag? If you have severe liver disease. Ezetimibe is metabolized by the liver, so your doctor may adjust your dose. Also, while rare, there have been isolated reports of liver enzyme elevations. If you notice yellowing skin, dark urine, or persistent nausea with fatigue, get checked.
Why Ezetimibe Still Matters in 2026
New drugs like bempedoic acid (Nexletol) and PCSK9 inhibitors are out there. But ezetimibe hasn’t been replaced. Why?- It’s cheap. At $0.11 per pill, it’s one of the most affordable options.
- It’s proven. The IMPROVE-IT trial showed it reduces heart attacks and strokes when added to statins.
- It’s tolerable. Fewer people quit because of side effects than with almost any other cholesterol drug.
It’s not perfect. But for the millions who can’t handle statins-or need a little extra help-it’s one of the best tools we have. And its GI profile? It’s among the most favorable in the entire class.
What’s Next?
The ENHANCE-2 trial, which finished enrolling in late 2024, is comparing ezetimibe directly to bempedoic acid in statin-intolerant patients. Results are due in mid-2026. We might get more data on which drug causes fewer GI issues. But for now, the evidence is clear: ezetimibe is gentle, effective, and worth sticking with-even if your stomach feels off at first.Does ezetimibe cause serious diarrhea?
Serious diarrhea is rare. Most cases are mild and last less than a month. Only about 0.7% of patients in clinical registries stop ezetimibe because of diarrhea. If you’re having frequent watery stools for more than 6 weeks, talk to your doctor-but don’t assume it’s the medication without ruling out other causes like infection or diet.
Can I take ezetimibe if I have IBS?
Yes, many people with IBS take ezetimibe without problems. Unlike statins, it doesn’t alter gut bacteria significantly. However, if you’re prone to diarrhea-predominant IBS, your doctor might start you on a lower dose or suggest taking it with food. Monitor your symptoms closely the first month.
Will ezetimibe make me gain weight?
No, ezetimibe has no known effect on weight. It doesn’t affect appetite, metabolism, or fat storage. Any weight changes while on the drug are likely due to diet, activity, or other medications.
Is it safe to take ezetimibe long-term?
Yes. Ezetimibe has been used safely for over 20 years. The FDA reaffirmed its safety profile in 2024, noting no new GI concerns in two decades of use. Long-term studies show it’s well-tolerated, with no increase in side effects over time.
Can I stop ezetimibe if my cholesterol improves?
Don’t stop without talking to your doctor. Cholesterol-lowering medications like ezetimibe work as long as you take them. Stopping can cause your LDL to rise again within weeks. Even if your numbers are good, continuing the drug helps maintain heart health long-term.











Lydia H.
19 Jan 2026 at 13:45Been on ezetimibe for 8 months now. Mild gas at first, like a tiny rebellious squirrel in my gut. Now? Nothing. Took two weeks. My doctor said it’s like training your intestines to stop panicking over less cholesterol. Honestly? Worth it for not having statin muscle pain.