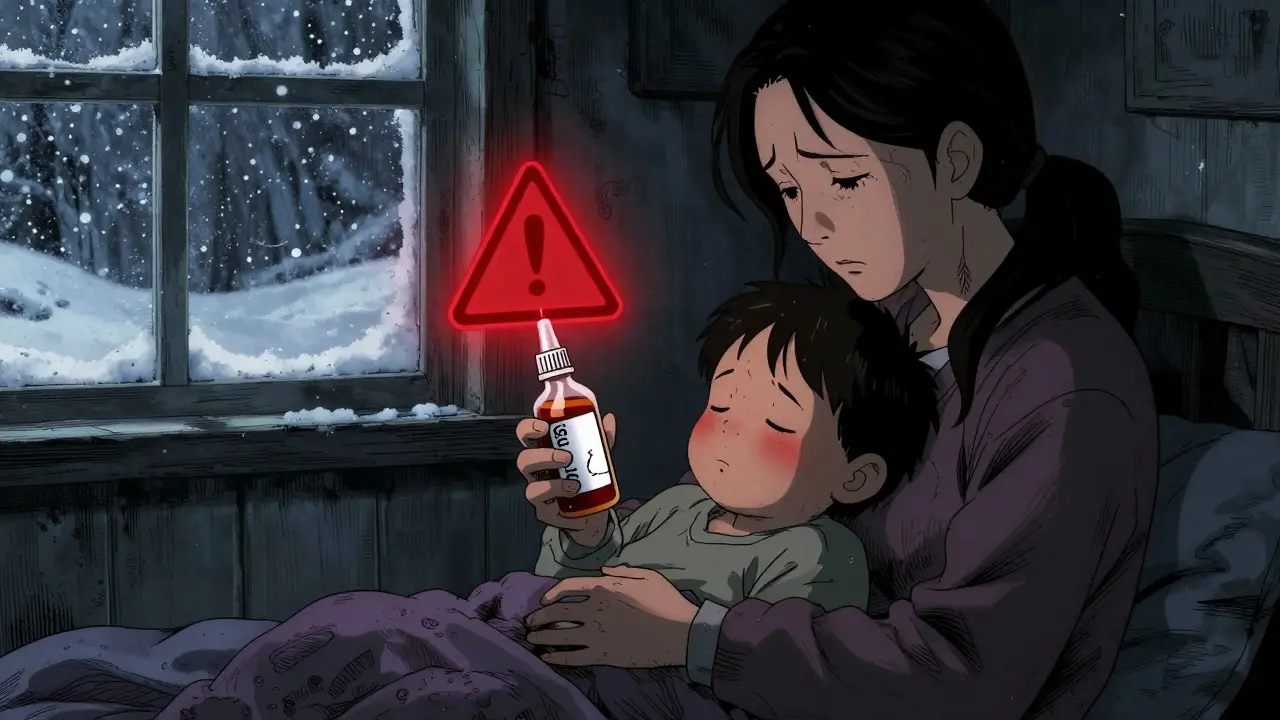
Every winter, parents face the same tough question: Should I give my child cough and cold medicine? It’s tempting. Your 3-year-old is coughing all night. Their nose is stuffed. You want to help them feel better. But the truth is, most over-the-counter cough and cold products aren’t just ineffective for kids under six-they can be dangerous.
The U.S. Food and Drug Administration (FDA) first warned parents in 2007 that these medications could cause serious harm in children under two. Since then, research has only strengthened that warning. Between 1969 and 2006, more than 120 deaths were linked to these products in young children. Even today, emergency rooms see thousands of cases each year from accidental overdoses, wrong dosing, or mixing medications. And here’s the kicker: there’s no solid proof these drugs actually work for kids under six.
Why These Medicines Don’t Work-and Can Hurt
Most children’s cough and cold products contain a mix of ingredients: antihistamines like chlorpheniramine, decongestants like pseudoephedrine, cough suppressants like dextromethorphan, and expectorants like guaifenesin. Sounds familiar? That’s because they’re the same as adult versions. But children’s bodies don’t process them the same way.
Young kids have underdeveloped liver enzymes. At age two, a child’s body has only about 23% of the enzyme activity needed to break down dextromethorphan safely. That means even a small dose can build up in their system. The result? Fast heartbeat, trouble breathing, seizures, or even coma. One study found that 67% of medication errors in kids under six came from incorrect dosing. Many parents used kitchen spoons instead of the measuring cup that came with the bottle. A teaspoon isn’t a milliliter. And that difference can be life-threatening.
Another big risk? Double-dosing. Parents don’t realize that many cold products contain acetaminophen. If you give your child a cough syrup with acetaminophen and then give them a separate fever reducer with the same ingredient, you’re overloading their liver. That can lead to liver failure. The FDA has documented cases where children ended up in intensive care because of this simple mistake.
What the Experts Say: Clear Age-Based Rules
The guidelines are simple-and they’re backed by every major medical group in the U.S. and Australia:
- Under 2 years: Never use OTC cough and cold medicine. The risk of serious side effects far outweighs any possible benefit.
- 2 to 4 years: Not recommended. The American Academy of Pediatrics says these medications aren’t effective and carry unnecessary risk.
- 4 to 6 years: Only use if your doctor specifically says so. Even then, stick to one product, one dose, and use the measuring tool that comes with it.
- 7 years and older: Can be used cautiously, following label instructions exactly.
The Mayo Clinic, Cincinnati Children’s Hospital, and Nationwide Children’s Hospital all agree: Don’t give these medicines to kids under six unless a doctor says it’s okay. The FDA still says the same thing in its 2023 update: the risks outweigh any benefit.

What Actually Works: Safe, Proven Alternatives
If not medicine, then what? The good news is, there are simple, safe, and effective ways to help your child feel better.
- Saline drops and suction: For babies and toddlers with a stuffy nose, saline nasal drops followed by gentle suction with a bulb syringe work wonders. Do this before feedings and bedtime.
- Cool-mist humidifier: Run one in your child’s room. Moist air helps loosen mucus and calm coughing. Never use a warm-mist humidifier-steam can burn kids or worsen nasal swelling.
- Honey: For children over one year old, a half to one teaspoon of honey before bed can reduce nighttime coughing better than some OTC cough syrups. A 2023 study from the American College of Chest Physicians called honey the first-line treatment for cough in kids over one. It thins mucus and soothes the throat. Just don’t give honey to babies under one-it can cause botulism.
- Hydration: Keep your child drinking water, breast milk, or formula. Fluids thin mucus and prevent dehydration.
- Acetaminophen or ibuprofen: If your child has a fever or body aches, you can use these pain relievers. But only if needed, and only at the right dose: 10-15 mg per kilogram of body weight every 4-6 hours. Never exceed five doses in 24 hours. Always check the label for acetaminophen content if you’re also using a cold medicine.
What Parents Still Get Wrong
Despite years of warnings, many parents still reach for OTC meds. A 2022 survey found that 42% of parents with kids under six still gave them cough and cold medicine. Why? They believed it would help their child feel better faster. But the data says otherwise.
Another dangerous habit? Using adult medicine. One in three parents admitted they’ve given their child adult cold medicine because they didn’t have a children’s version on hand. That’s a huge risk. Adult doses can be 3-5 times too strong for a toddler. The FDA warns this practice can lead to overdose, hallucinations, or even death.
And then there’s the myth of “just one more.” Parents think, “I already gave it at 8 a.m., but it’s not working. I’ll give it again.” That’s how accidental overdoses happen. These medicines don’t work faster with more doses. They just build up to toxic levels.

What’s Changing-and What’s Next
Manufacturers have responded to safety concerns. Since 2008, most products now carry labels saying “Do not use in children under 4.” But a 2021 FDA inspection found that 22% of products still didn’t have clear warnings. That means you still need to read every label carefully.
Public health campaigns are working. Between 2005 and 2011, emergency visits for OTC medication reactions in kids under two dropped by 45%. But disparities remain. Black and Hispanic children are still more likely to be treated for these reactions, likely due to limited access to healthcare advice and affordable alternatives.
Now, research is shifting focus. A 2023 study in JAMA Pediatrics showed that when parents received clear, simple education about safe symptom management, inappropriate OTC use dropped by 58%. That’s huge. It proves that with the right information, parents make safer choices.
Bottom Line: Less Medicine, More Care
You love your child. You want to fix their cough. But the truth is, most colds are viruses. They run their course. Medicine won’t speed that up. And the wrong medicine might make things worse.
Stick to the basics: saline, honey (if over one), hydration, and rest. Use acetaminophen or ibuprofen only for fever or pain. Never mix products. Never use adult medicine. Always measure with the tool that comes with the bottle.
If your child has trouble breathing, a fever over 38.5°C for more than 72 hours, or seems unusually sleepy or irritable-call your doctor. Don’t wait. Don’t guess. And don’t reach for the medicine cabinet without knowing what’s inside.
For kids under six, the safest cough and cold remedy isn’t in a bottle. It’s in your arms, your patience, and your knowledge.
Can I give my 3-year-old Children’s Dimetapp or similar OTC medicine?
No. The American Academy of Pediatrics, FDA, and other major health groups strongly advise against giving OTC cough and cold medicines to children under 4. These products contain ingredients like dextromethorphan and antihistamines that can cause serious side effects-including rapid heart rate, seizures, and breathing problems-even at recommended doses. A 2023 study found that 38% of parents who gave these medicines to toddlers reported unexpected side effects like hyperactivity or sleeplessness. Stick to saline drops, honey (if over 1 year), and a humidifier instead.
Is honey really safe for toddlers with cough?
Yes-for children over one year old. Honey is a proven cough suppressant. A 2023 review from the American College of Chest Physicians found honey works as well as, or better than, many OTC cough medicines for reducing nighttime coughing in kids. Give ½ to 1 teaspoon before bed. But never give honey to babies under one. It can cause infant botulism, a rare but serious illness.
What should I do if my child has a fever and a runny nose?
Use acetaminophen or ibuprofen only if your child is uncomfortable or has a fever over 38.5°C. Don’t give them just because they have a cold. For the runny nose, use saline nasal drops and a bulb syringe to clear mucus. Keep them hydrated. Avoid combination cold medicines-many contain acetaminophen already. If you give a pain reliever and a cold medicine together, you risk giving too much acetaminophen, which can damage the liver.
Can I use adult cold medicine if I don’t have children’s medicine?
Never. Adult cold medicines contain much higher doses of active ingredients. Giving even a small amount to a toddler can lead to overdose. The FDA has documented cases of children going into emergency rooms after parents used adult formulations. If you don’t have children’s medicine, don’t guess. Use saline, honey, and a humidifier instead. Call your doctor if symptoms worsen.
Are humidifiers safe for young children?
Yes-but only cool-mist humidifiers. Warm-mist humidifiers can cause burns or worsen nasal swelling. Clean the humidifier daily to prevent mold and bacteria buildup. Use distilled or boiled water if possible. Place it near your child’s bed but out of reach. Humid air helps loosen mucus and makes breathing easier, especially at night.
How do I know if my child needs to see a doctor?
Call your doctor if your child has trouble breathing, a fever lasting more than 72 hours, is unusually sleepy or irritable, refuses to drink, or has a cough that sounds like a seal barking (possible croup). Also call if your child is under 3 months old with any fever. Most colds are viral and go away on their own, but these signs could mean something more serious.










Write a comment