Corticosteroid Psychosis Risk Calculator
Calculate Your Risk
Estimate your risk of developing psychiatric symptoms while taking corticosteroids based on key factors.
Risk Assessment
Based on your input, your risk of developing psychiatric symptoms is:
Key Risk Factors
Recommendations
When you’re prescribed corticosteroids-whether for asthma, rheumatoid arthritis, or a flare-up of an autoimmune condition-you’re usually told about the common side effects: weight gain, increased blood sugar, or trouble sleeping. But there’s another side effect that rarely gets mentioned, even though it can turn your life upside down: psychosis.
It sounds extreme, but it’s real. In fact, up to 18% of people taking high-dose corticosteroids develop serious psychiatric symptoms. That’s not a rare fluke. It’s a predictable risk tied directly to the dose. And it doesn’t just affect older adults or those with a history of mental illness. It can hit anyone, even someone who’s never had a single panic attack in their life.
How High Is the Risk?
The numbers don’t lie. At doses under 40 mg of prednisone per day, the chance of developing psychiatric symptoms is around 1.3%. But when the dose jumps to 80 mg or higher? That risk shoots up to 18.4%. That’s nearly one in five people. And since doctors in the U.S. write about 10 million new oral corticosteroid prescriptions every year, we’re talking about tens of thousands of people each year who could experience mood swings, mania, or full-blown psychosis.
It’s not just about the dose. Timing matters too. Symptoms often show up within the first few days-sometimes as early as day two or three. The median onset? Three to four days after starting treatment. That means if you’re on a high-dose taper, the worst of it might hit right when you think you’re finally getting better.
What Do These Changes Look Like?
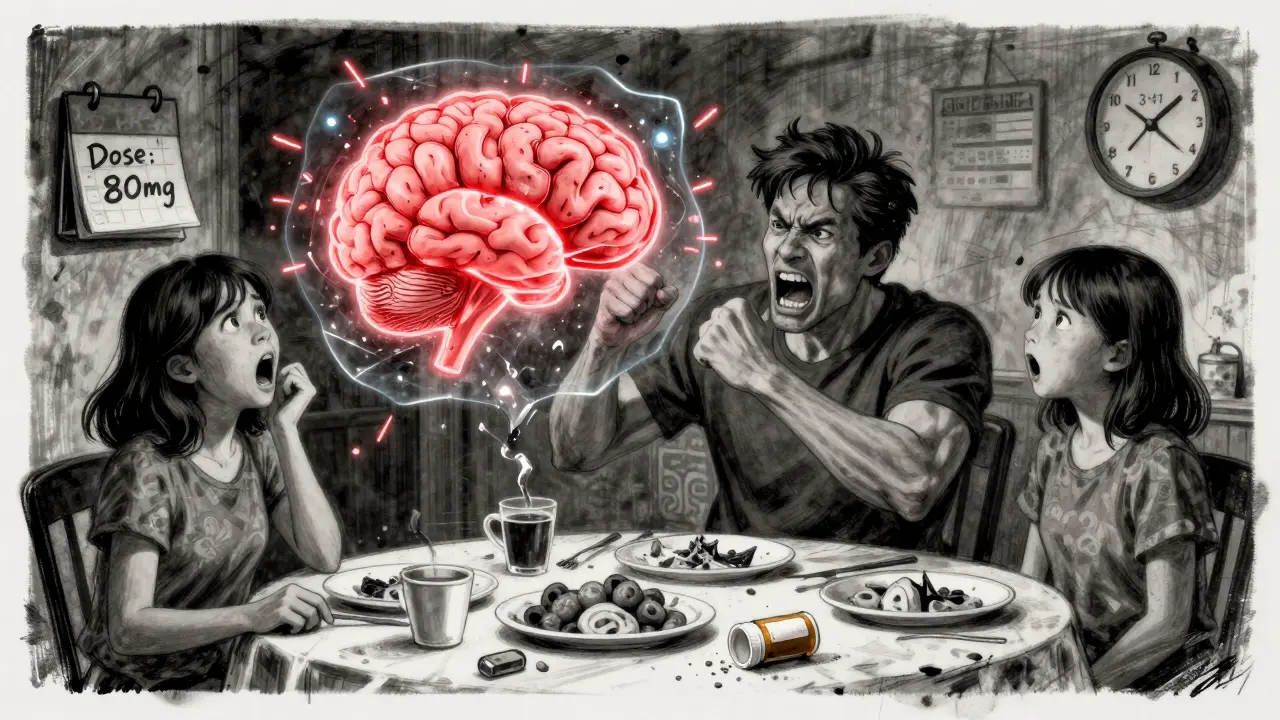
Psychosis isn’t always screaming at imaginary voices. It can start quietly. You might notice:
- Sudden, unexplained euphoria-feeling oddly happy or invincible when nothing in your life justifies it.
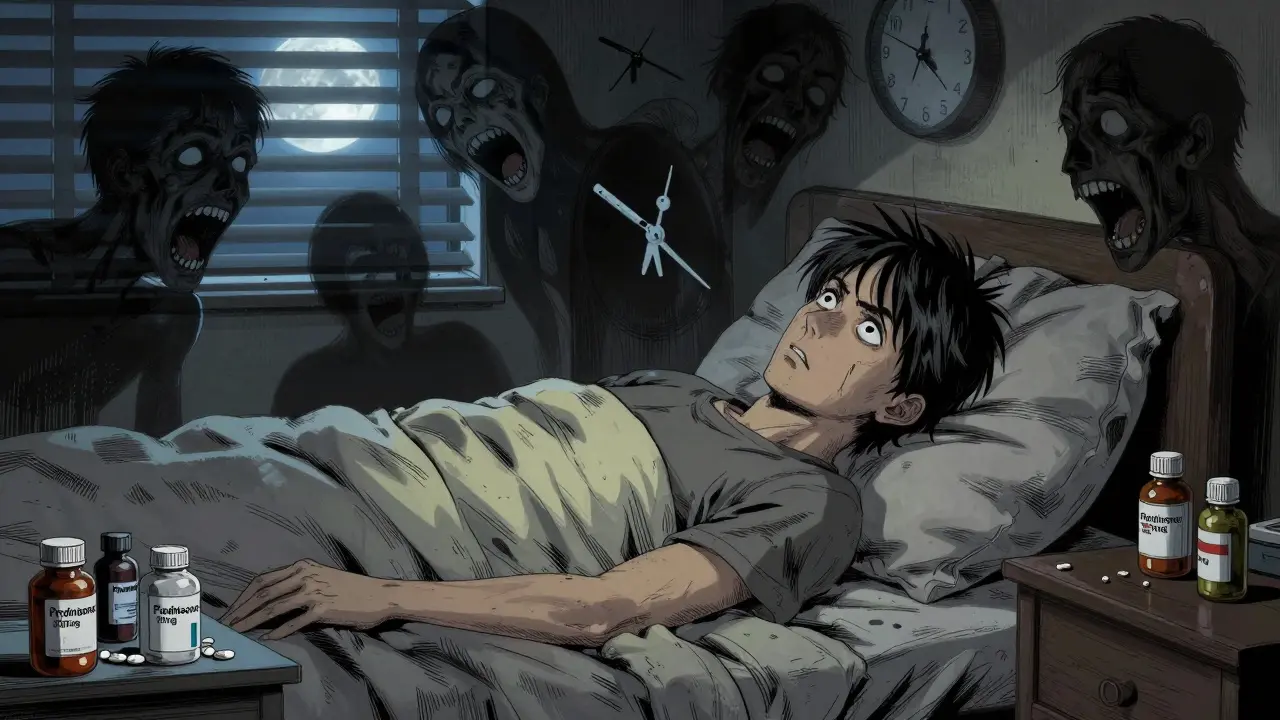
- Insomnia that won’t quit, even when you’re exhausted.
- Mood swings that feel like a rollercoaster: one minute you’re calm, the next you’re furious over a spilled cup of coffee.
- Personality shifts-someone who’s usually easygoing becomes suspicious, withdrawn, or aggressive.
- Severe depression, with thoughts of worthlessness or hopelessness that don’t match your situation.
- Delusions or hallucinations: believing things that aren’t true, seeing things that aren’t there, or hearing voices.
Memory problems are common too. People report struggling to remember names, appointments, or even what they had for breakfast. It’s not just forgetfulness-it’s a noticeable dip in verbal and declarative memory, linked to how corticosteroids affect the hippocampus.
And here’s the twist: you don’t need to have all these symptoms. One study found that 11.8% of cases presented with mania alone, while 23.5% had psychosis without any manic symptoms. So if you’re only feeling unusually elated or unusually paranoid, it still counts.
Who’s Most at Risk?
It’s not random. Certain factors make some people far more vulnerable:
- High doses-anything above 40 mg of prednisone daily is a red flag.
- Older age-people over 65 are at higher risk, likely due to changes in brain chemistry and metabolism.
- Female sex-multiple studies show women are more susceptible than men, though the reason isn’t fully understood.
- Pre-existing mental illness-especially bipolar disorder. If you’ve had manic episodes before, corticosteroids can trigger a full relapse.
- Prolonged use-the longer you’re on it, the higher the chance of symptoms sticking around.
Even more concerning: symptoms can last after you stop taking the drug. Case reports show mania and psychosis persisting for weeks-or even months-after corticosteroid discontinuation. That’s not a temporary glitch. It’s a neurological ripple that takes time to settle.

Why Does This Happen?
We don’t have all the answers, but science has a few strong clues:
- HPA axis suppression-corticosteroids shut down your body’s natural stress response system. That throws off your cortisol rhythm, which affects mood regulation.
- Hippocampal impact-this brain region, critical for memory and emotion, is sensitive to high levels of glucocorticoids. Animal studies show structural changes after prolonged exposure.
- Dopamine surge-in lab models, corticosteroids boost tyrosine hydroxylase, an enzyme that ramps up dopamine production. Too much dopamine? That’s a known pathway to psychosis.
It’s likely a mix of all three. That’s why symptoms vary so much from person to person. One person gets insomnia and irritability. Another spirals into delusions. The same drug, different brain responses.
What Should You Do If You Notice Changes?
If you or a loved one starts acting strangely while on corticosteroids, don’t wait. Don’t assume it’s just stress or fatigue. Don’t brush it off as "just being moody." Here’s what to do:
- Check the dose. Are you on more than 40 mg of prednisone (or equivalent)? If yes, that’s a major risk factor.
- Track symptoms. Write down changes in mood, sleep, memory, or behavior. Note when they started and how they’ve changed.
- Contact your doctor immediately. Don’t wait for your next appointment. Call your prescriber or go to urgent care.
- Don’t stop cold turkey. Abruptly stopping corticosteroids can be dangerous. Tapering must be done under medical supervision.
The good news? Most people get better. About 92% of patients see full symptom resolution once the dose is lowered below 40 mg/day. But that only works if you catch it early.
How Is It Treated?
There’s no FDA-approved drug specifically for corticosteroid-induced psychosis. That’s a huge gap. But doctors have learned what works through trial and case reports:
- Tapering the steroid is always step one. If possible, reduce to under 40 mg/day of prednisone (or 6 mg of dexamethasone).
- Low-dose antipsychotics are often used off-label: haloperidol (0.5-1 mg/day), risperidone (1-4 mg/day), or olanzapine (2.5-20 mg/day). Symptoms usually improve within days to weeks.
- Lithium has been used to prevent mania, but it’s risky-kidney and thyroid side effects make it a last-resort option.
- Psychiatry consultation is critical. This isn’t just a "doctor’s problem." It needs a team: your rheumatologist, pulmonologist, and a psychiatrist working together.
Diagnosis is tricky. Doctors must rule out everything else: drug interactions, infections, metabolic imbalances, brain tumors, or other psychiatric illnesses. Steroid-induced psychosis is a diagnosis of exclusion. That means if you’re not getting better, you need a deeper dive.
What’s Missing in Clinical Practice?
Here’s the uncomfortable truth: we’re still flying blind in many ways.
- There’s no standard screening tool for these symptoms.
- Most patient education materials don’t mention psychosis at all.
- Pharmacists, nurses, and primary care providers often aren’t trained to recognize early signs.
- Even when symptoms are noticed, they’re frequently mislabeled as "anxiety" or "non-compliance."
Experts are calling for "clinimetric methods"-better tools to measure severity and track changes over time. Right now, we’re relying on anecdotal reports and guesswork.
And while we’ve known about this for over 70 years, no targeted treatment has been developed. No new drugs. No clinical trials. Just off-label patches stitched together from case reports.
What You Can Do Now
If you’re on corticosteroids:
- Ask your doctor: "What are the psychiatric risks at my dose?"
- Ask your pharmacist: "Should I be watching for mood or memory changes?"
- Set up a daily mood check: rate your sleep, irritability, and focus on a scale of 1-10.
- Tell a close family member what to look for. They’ll notice changes before you do.
- Keep a log. Write down when symptoms started, what you were taking, and how you felt.
If you’re a caregiver or family member: if someone on steroids suddenly becomes paranoid, aggressive, or detached from reality, don’t assume it’s "just stress." It could be the medication.
There’s no shame in this. Corticosteroids save lives. But they’re not harmless. Understanding the full picture-especially the hidden mental health risks-is the only way to stay safe while getting the treatment you need.
Can corticosteroids cause psychosis even if I’ve never had mental health issues before?
Yes. Many people who develop corticosteroid-induced psychosis have no prior psychiatric history. The risk is tied to the dose and how your brain responds to the drug-not to past mental illness. Even healthy individuals on high doses can experience hallucinations or delusions.
How long do steroid-induced psychiatric symptoms last?
For most people, symptoms improve within days to weeks after lowering the dose or stopping the medication. But in some cases, especially with prolonged high-dose use, symptoms can persist for weeks or even months after discontinuation. This suggests corticosteroids may cause lasting changes in brain chemistry that take time to reverse.
Is there a blood test to check for steroid-induced psychosis?
No. There’s no blood test, brain scan, or biomarker that can confirm steroid-induced psychosis. Diagnosis is based on clinical observation: timing of symptoms relative to steroid use, ruling out other causes, and response to dose reduction. That’s why it’s often missed or misdiagnosed.
Can I still take corticosteroids if I have a history of depression?
You can, but with extreme caution. If you have a history of depression or bipolar disorder, your doctor should consider lower doses, shorter courses, and close psychiatric monitoring. In some cases, preventive mood stabilizers like lithium may be considered-but only under specialist supervision due to risks.
Are inhaled or topical steroids safe from psychiatric side effects?
Inhaled and topical corticosteroids rarely cause psychiatric side effects because very little of the drug enters your bloodstream. The risk is almost entirely tied to systemic (oral or IV) use. If you’re using an inhaler or cream, you don’t need to worry about psychosis or mood swings.
If you’re currently on corticosteroids and feeling off-not just physically, but mentally-don’t ignore it. Talk to your doctor. Keep track. Know the signs. This isn’t just about managing a disease. It’s about protecting your mind while you heal your body.






Charlotte Dacre
14 Feb 2026 at 06:19So let me get this straight - we’re giving people a drug that can turn them into a chaotic, delusional mess, but we don’t screen for it? And we wonder why people think doctors are just ‘out of touch’? 😏
My aunt was on prednisone for lupus. One day she was baking cookies, the next she was convinced the mailman was stealing her thoughts. She didn’t even remember calling 911 because ‘the fridge was talking.’
Doctors just shrugged and said ‘stress.’
Turns out, it was the steroids. Took three weeks after stopping for her to stop accusing the cat of being a government spy.
Why isn’t this on the prescription label? Like, right under ‘may cause weight gain’? ‘Also may cause you to yell at your toaster’?
I’m not mad… I’m just disappointed.