DRESS syndrome isn’t just a rash. It’s a full-body alarm triggered by a medication your body treats like an invader. If you’ve been on a new drug for a few weeks and suddenly feel sick, break out in a widespread rash, and your fever won’t break - this could be it. DRESS (Drug Reaction with Eosinophilia and Systemic Symptoms) kills about 1 in 10 people who don’t get help fast enough. But if caught early, survival rates jump to over 95%. The problem? Most doctors miss it.
What DRESS Actually Looks Like
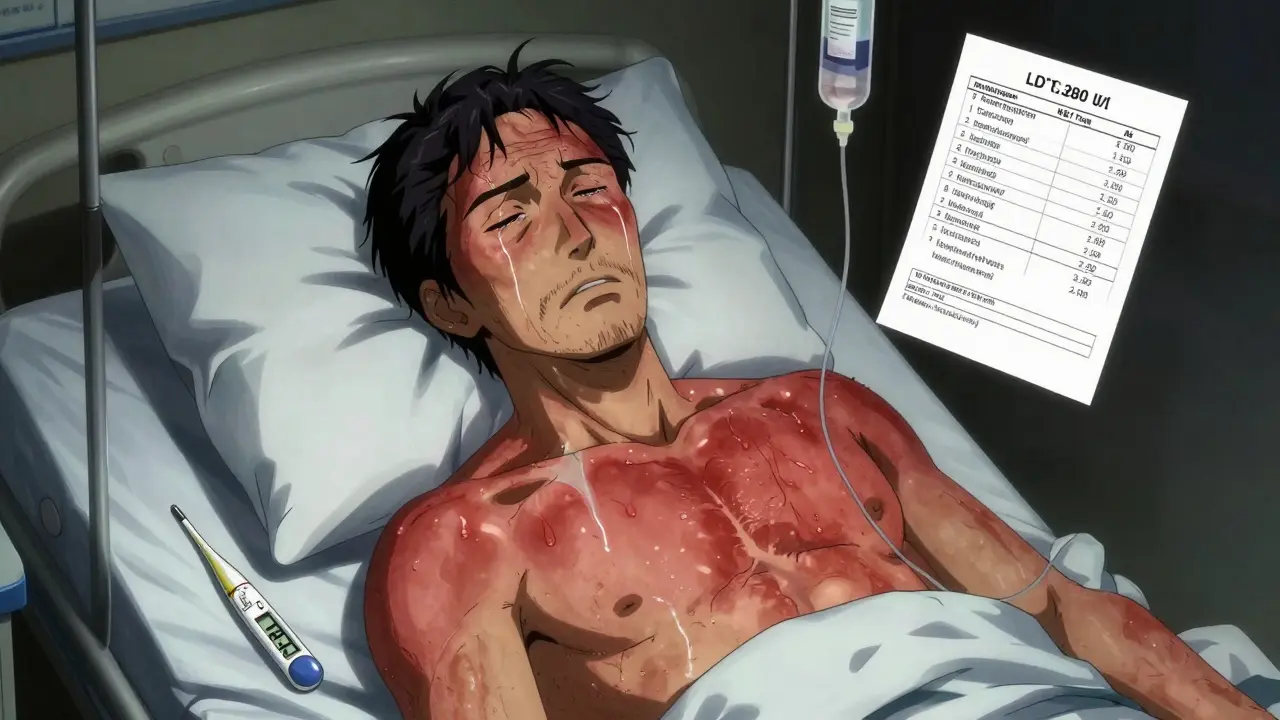
DRESS doesn’t start with a few spots. It begins with something that feels like the flu: fatigue, sore throat, swollen glands, and a fever over 38°C. Within a day or two, a red, flat, measles-like rash spreads across your chest, back, and face. It’s not itchy at first - that’s why people ignore it. By the time it becomes painful or blisters, it’s often too late.
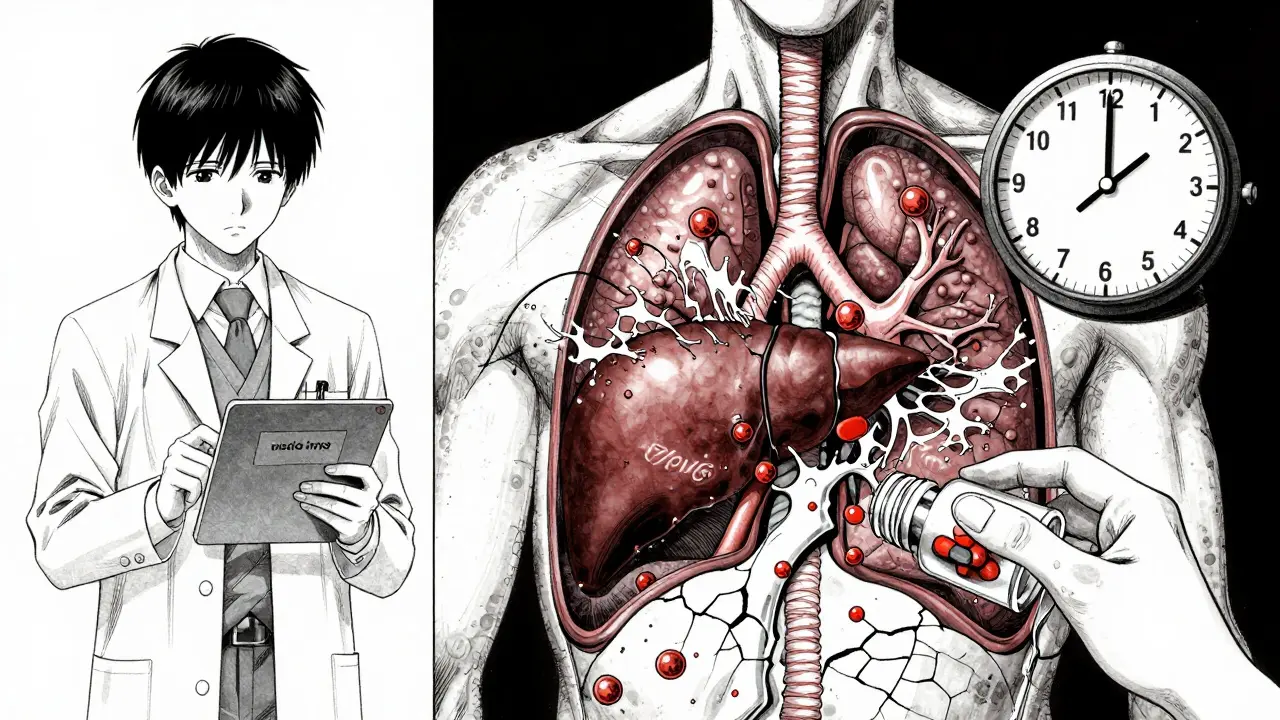
What makes DRESS dangerous isn’t just the skin. Your liver, kidneys, lungs, heart, or pancreas can start failing - quietly. Liver damage is the most common. ALT levels above 1,000 U/L aren’t rare. One patient in Melbourne had levels hit 2,840 U/L after starting allopurinol for gout. He spent 45 days in hospital. Most people don’t realize their fever and rash are linked to a pill they took six weeks ago.
Which Drugs Trigger DRESS?
Not every drug causes this. But some are well-known culprits. Allopurinol - the most common offender - triggers nearly half of all cases. It’s usually prescribed for gout or high uric acid. The risk spikes if you have kidney disease. If your eGFR is below 60, your chance of DRESS jumps from 1 in 10,000 to 1 in 200.
Antiepileptic drugs like carbamazepine, phenytoin, and lamotrigine are next. These are used for seizures, bipolar disorder, or nerve pain. Sulfonamide antibiotics like Bactrim are also high-risk. Even some antivirals and NSAIDs have been linked.
The delay is the trick. Unlike allergic reactions that hit minutes after a pill, DRESS takes 2 to 8 weeks. Some cases appear as late as 16 weeks. That’s why it’s so often misdiagnosed as a virus, heat rash, or even a new infection.
DRESS vs. Other Drug Rashes
Stevens-Johnson Syndrome (SJS) and Toxic Epidermal Necrolysis (TEN) are also deadly skin reactions. But they’re different. SJS/TEN hit faster - within 1 to 4 weeks. They cause massive skin peeling, like a burn. Mucous membranes in your mouth, eyes, and genitals are almost always destroyed.
DRESS? Skin peeling is rare. Mucosal damage happens in only 30-50% of cases. The real giveaway? Eosinophils. These are white blood cells that normally fight parasites. In DRESS, they surge above 1,500 per microliter - sometimes over 5,000. You’ll also see atypical lymphocytes, swollen lymph nodes, and organ damage. SJS/TEN don’t show this pattern.
And here’s the kicker: up to 70% of DRESS patients reactivate HHV-6 - a herpes virus most people carry silently. That reactivation might be why symptoms linger for months, even after stopping the drug.

How Doctors Diagnose It
There’s no single blood test for DRESS. Diagnosis relies on a checklist called the RegiSCAR criteria. You need to be hospitalized, plus at least three of these:
- Fever above 38°C
- Skin rash
- Swollen lymph nodes
- Eosinophils over 1,500/μL or more than 10% of white blood cells
- Atypical lymphocytes in blood
- One or more internal organs affected (liver, kidney, lung, heart)
Doctors also check for HHV-6 DNA in blood - if it’s high, it supports the diagnosis. Liver enzymes, kidney function, and full blood counts are tracked daily. Many patients are misdiagnosed because their doctor doesn’t ask about medications from six weeks ago. One study found only 35% of internal medicine residents could correctly identify DRESS.
What Happens If You Don’t Act
Delaying treatment raises your death risk from 5% to 15%. The biggest killer is liver failure. Hepatic necrosis - massive death of liver cells - can happen fast. Kidney failure, pneumonia, and sepsis from secondary infections are also common. About 10% of patients develop bacterial or fungal infections in their bloodstream, including MRSA or Candida.
Even if you survive, you’re not out of the woods. Between 20% and 30% of survivors have lasting organ damage. Kidney problems are the most frequent. One survey of 150 DRESS survivors found 27% needed ongoing nephrology care. Some develop autoimmune diseases months later - like Graves’ disease or lupus - because the immune system stays scrambled.
How It’s Treated
The first step? Stop the drug - immediately. Don’t wait for test results. If you suspect DRESS, call your doctor or go to the ER. If you’re on allopurinol and develop a rash with fever, stop it now. That single action cuts your death risk in half.
Most patients need hospitalization for 14 to 21 days. Treatment usually includes high-dose steroids like prednisone or methylprednisolone (1 mg per kg of body weight daily). The dose is slowly lowered over 4 to 8 weeks. Too fast, and symptoms can rebound. Too slow, and you risk side effects like bone loss or diabetes.
For severe cases that don’t respond to steroids, newer drugs are being tested. Anakinra - a drug used for rheumatoid arthritis - has shortened hospital stays by over a week in trials. Tocilizumab, another immune blocker, is now in phase II trials. These aren’t standard yet, but they’re promising.
Infection control is critical. Patients are often isolated. IV antibiotics or antifungals are used if infection is suspected. Blood cultures, chest X-rays, and ultrasounds of the liver and kidneys are routine.
Who’s at Highest Risk?
It’s not random. Genetics matter. People with the HLA-B*58:01 gene variant are 55 times more likely to get DRESS from allopurinol. This variant is common in East Asian, Southeast Asian, and African populations. That’s why Taiwan now requires genetic testing before prescribing allopurinol. Since 2020, DRESS cases from allopurinol dropped by 75% there.
Age and kidney health are big factors. Most cases occur in adults over 40. If you have chronic kidney disease (eGFR under 60), your risk is sky-high. That’s why the American College of Rheumatology now recommends febuxostat instead of allopurinol for patients with kidney impairment.
Even if you’re young and healthy, don’t assume you’re safe. DRESS can strike anyone on a high-risk drug - even if you’ve taken it before without issues.
What to Do If You’re Taking High-Risk Drugs
If you’re on allopurinol, carbamazepine, lamotrigine, or sulfonamides:
- Know the warning signs: fever, rash, swollen glands, fatigue
- Track when you started the drug - DRESS happens 2-8 weeks later
- If you develop a rash with fever, stop the drug and seek help immediately
- Ask your doctor about HLA-B*58:01 testing if you’re of Asian descent or have kidney disease
- Keep a list of all medications - including over-the-counter and supplements
Don’t wait for a second opinion. If your GP says it’s just a virus or allergy, push for a referral to a dermatologist or immunologist. The DRESS Syndrome Foundation has a patient navigator program that helps people cut through diagnostic delays - 85% of users say it saved them weeks of confusion.
Long-Term Outlook
Most people recover fully if treated early. But recovery takes time. Skin can take months to return to normal. Fatigue and joint pain linger for some. Regular follow-ups for liver and kidney function are essential for at least a year.
Some patients develop new autoimmune conditions. If you had DRESS from carbamazepine and later feel shaky, lose weight, or have a rapid heartbeat - get your thyroid checked. It’s not coincidence. About 5-10% of survivors develop autoimmune thyroid disease, type 1 diabetes, or lupus.
The good news? Awareness is rising. ICD-10 billing for DRESS has quadrupled since 2015. More doctors are learning to recognize it. But you still need to be your own advocate.
If you’ve had a recent rash after starting a new medication - especially if you’re over 40, have kidney issues, or are on allopurinol - don’t brush it off. DRESS doesn’t wait. Neither should you.






Alec Amiri
22 Jan 2026 at 05:29Bro. This is wild. I had a rash after allopurinol and thought it was heat. Turned out I was one step from liver failure. Docs didn't even ask about meds. Stop the pill. Go to ER. Don't wait.