When you're taking azilsartan for high blood pressure, you probably don't think about your liver. That’s normal. Most people focus on how well their blood pressure is controlled, not how their body processes the drug. But here’s something most don’t ask: azilsartan and liver function do connect - and it’s not as simple as "it’s safe" or "it’s risky."
What is azilsartan, really?
Azilsartan is an angiotensin II receptor blocker (ARB), a class of drugs used to lower blood pressure. It works by blocking a hormone that tightens blood vessels, letting them relax and reducing pressure on the heart. It’s not new - approved by the FDA in 2011 - but it’s still less commonly prescribed than losartan or valsartan. That doesn’t mean it’s less effective. In fact, clinical trials showed azilsartan lowers systolic blood pressure more than olmesartan in some patients, especially those with resistant hypertension.
It’s taken once daily, usually in doses of 20 mg to 80 mg. Most people tolerate it well. But like all medications, it’s processed through the body - and that includes the liver.
How the liver handles azilsartan
Your liver doesn’t break down azilsartan the same way it handles other blood pressure drugs. Unlike some ARBs that rely heavily on liver enzymes like CYP3A4, azilsartan is mostly eliminated unchanged through the kidneys. Only about 20% is metabolized in the liver, mainly by esterases - enzymes that aren’t part of the classic drug-metabolizing system.
This matters because if your liver is already damaged, many drugs build up and cause harm. But azilsartan’s low liver metabolism means it’s less likely to pile up in people with mild to moderate liver disease. That’s a key point: azilsartan isn’t processed like statins, acetaminophen, or even some other ARBs. It’s gentler on the liver by design.
Can azilsartan damage your liver?
There’s no strong evidence that azilsartan causes liver injury in healthy people. In clinical trials involving over 4,000 patients, liver enzyme elevations (like ALT or AST) were no more common with azilsartan than with placebo. That’s unusual. Most drugs, even safe ones, show slight, harmless spikes in liver enzymes in a small percentage of users. Azilsartan doesn’t even do that consistently.
There have been fewer than five reported cases of drug-induced liver injury linked to azilsartan in global databases since its launch. None were severe. In each case, patients had other risk factors - like alcohol use, pre-existing liver disease, or were taking multiple medications that stress the liver.
Bottom line: azilsartan is not a known hepatotoxin. If your liver is healthy, you don’t need to worry about it harming your liver.
What if you already have liver disease?
Here’s where things get practical. If you have cirrhosis, hepatitis, fatty liver disease, or any chronic liver condition, your doctor might still prescribe azilsartan - but with caution. Why? Because even though the liver doesn’t break it down much, your body’s overall ability to handle drugs changes when your liver is damaged.
Studies show that people with moderate to severe liver impairment (Child-Pugh Class B or C) may have slightly higher blood levels of azilsartan. Not enough to be dangerous, but enough that your doctor might start you on a lower dose - maybe 20 mg instead of 40 mg. They’ll also monitor your blood pressure and kidney function more closely, since the kidneys take over more of the work when the liver can’t help.
One thing to avoid: don’t start azilsartan if you have severe liver disease and are already on diuretics or have low blood pressure. That combo can cause your blood pressure to drop too far, leading to dizziness or fainting.
Signs your liver might be reacting
Even if azilsartan rarely causes liver problems, you should still know the warning signs. They’re not specific to azilsartan - they’re signs of any drug-related liver stress:
- Unexplained fatigue that doesn’t go away
- Yellowing of the skin or eyes (jaundice)
- Dark urine
- Abdominal pain, especially in the upper right side
- Nausea or vomiting that isn’t linked to food
- Itchy skin without a rash
If you notice any of these after starting azilsartan, don’t panic. But don’t ignore them either. Call your doctor. They’ll check your liver enzymes with a simple blood test. If levels are normal, it’s likely not the drug. If they’re high, they’ll consider stopping azilsartan or switching you to another ARB like telmisartan, which also has low liver metabolism.
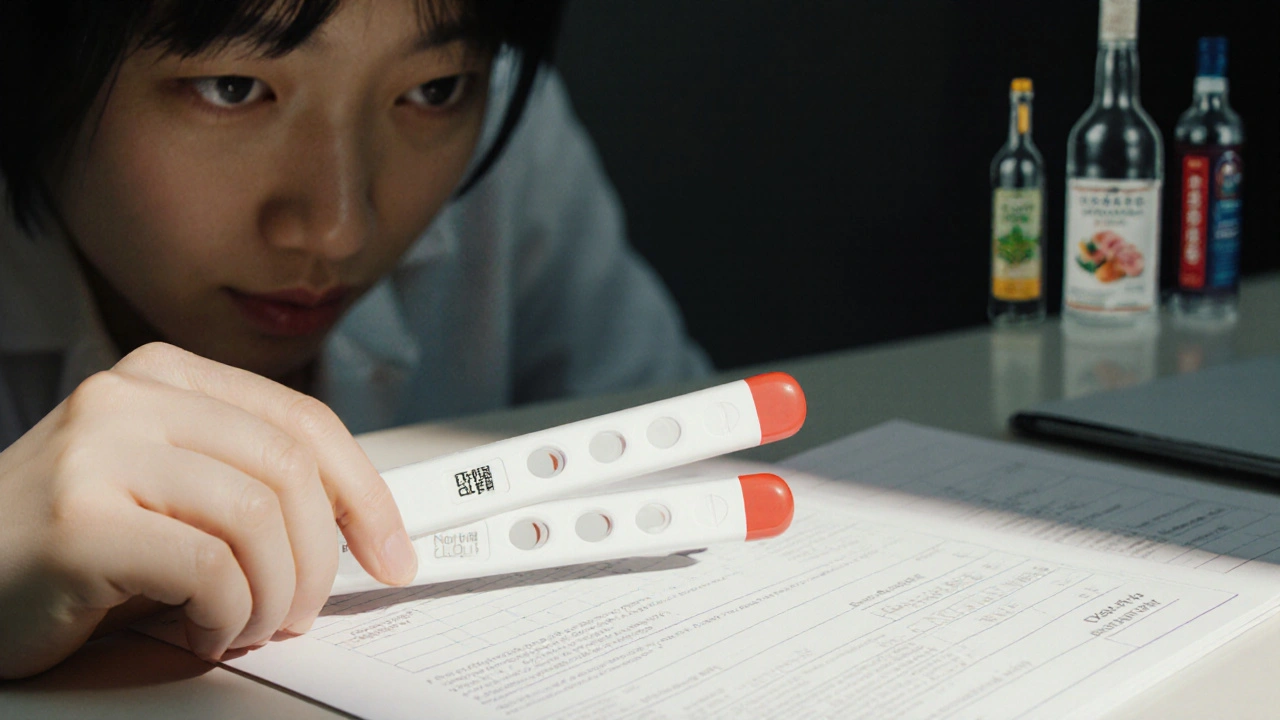
Testing liver function while on azilsartan
For most people, routine liver tests aren’t needed. The FDA doesn’t require them. Neither do major hypertension guidelines from the American Heart Association or European Society of Cardiology.
But if you have:
- Chronic liver disease
- History of alcohol abuse
- Been on multiple medications for years
- Are over 65 with other health conditions
Then your doctor may order a baseline liver panel before starting azilsartan - and repeat it in 3 to 6 months. After that, annual checks are usually enough unless something changes.
There’s no magic number that says "stop the drug." But if ALT or AST levels rise above three times the upper limit of normal, that’s when doctors start looking for causes - including azilsartan.
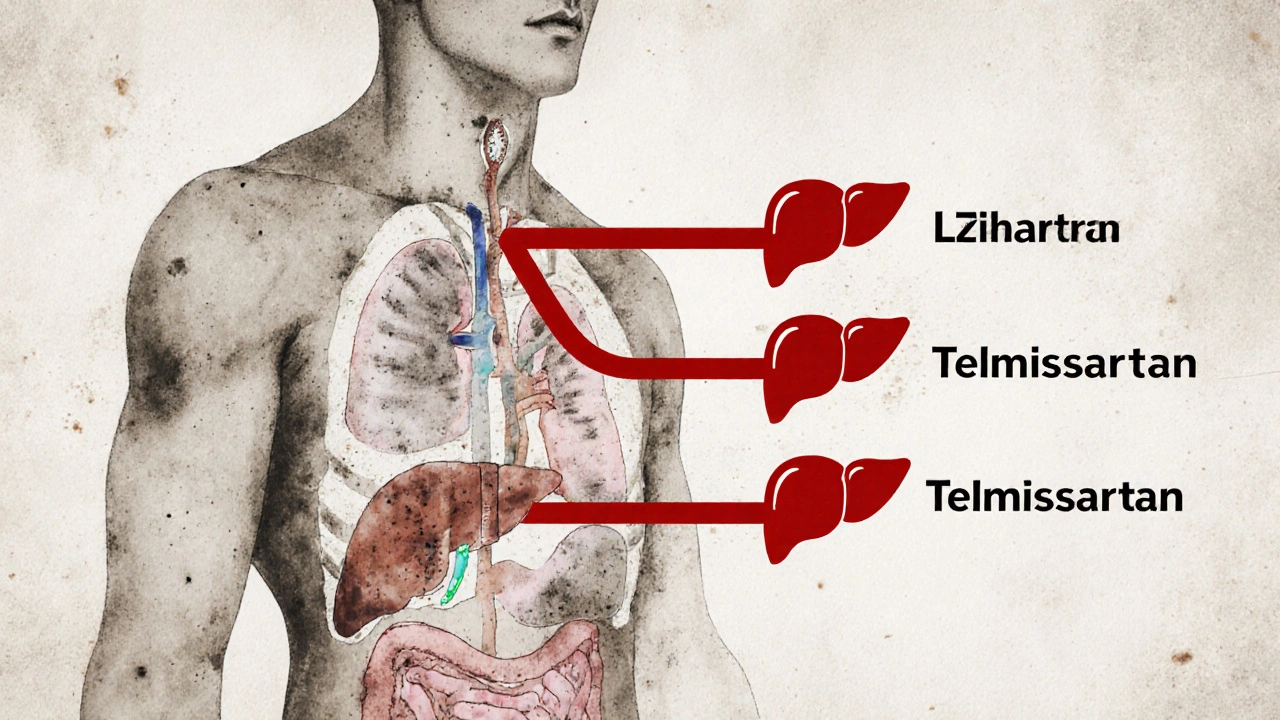
How azilsartan compares to other ARBs
Not all blood pressure drugs are the same when it comes to liver safety. Here’s how azilsartan stacks up:
| Medication | Primary Metabolism Pathway | Common Liver Enzyme Elevations | Recommended in Mild Liver Disease? | Severe Liver Disease Caution? |
|---|---|---|---|---|
| Azilsartan | Renal excretion (20% liver esterases) | Very rare | Yes | Yes - lower dose |
| Losartan | CYP2C9 liver metabolism | Mild, occasional | Yes | Yes - avoid if severe |
| Valsartan | Minor liver metabolism | Rare | Yes | Yes - monitor |
| Telmisartan | High liver metabolism (CYP2C9) | Occasional | Yes | Yes - avoid if severe |
| Candesartan | Minor liver metabolism | Rare | Yes | Yes - monitor |
As you can see, azilsartan and valsartan are the safest bets if liver health is a concern. Telmisartan, despite being effective, is metabolized more by the liver - so it’s riskier if you have cirrhosis.
What to do if you’re worried
If you’re on azilsartan and you’re anxious about your liver:
- Don’t stop taking it without talking to your doctor. Stopping suddenly can cause your blood pressure to spike.
- Ask for a liver enzyme test if you haven’t had one in the past year.
- Limit alcohol. Even moderate drinking can stress your liver while you’re on medication.
- Review all your supplements. Some herbs - like kava, green tea extract, or high-dose niacin - can harm the liver on their own.
- Keep your weight in check. Fatty liver disease is common in people with high blood pressure - and it makes liver monitoring more important.
Bottom line: Is azilsartan safe for your liver?
Yes - for nearly everyone. Azilsartan has one of the cleanest liver safety profiles among blood pressure medications. It doesn’t rely on the liver to work, doesn’t commonly raise liver enzymes, and rarely causes harm. Even if you have mild liver disease, it’s often a better choice than alternatives.
That doesn’t mean ignore your liver. If you have advanced liver disease, heavy alcohol use, or are on other liver-stressing drugs, talk to your doctor. They can tailor your treatment. But for most people, azilsartan is a quiet, reliable option - and your liver won’t even notice it’s there.
Can azilsartan cause elevated liver enzymes?
Rarely. In clinical trials, azilsartan caused liver enzyme elevations no more often than a placebo. Less than 1% of users showed any increase, and those were mild and temporary. It’s not a known cause of drug-induced liver injury in healthy individuals.
Is azilsartan safe if I have fatty liver disease?
Yes, it’s generally safe. Fatty liver disease doesn’t interfere with how azilsartan is processed. Since it’s mostly cleared by the kidneys, it doesn’t add stress to the liver. In fact, controlling blood pressure can help reduce liver inflammation over time.
Should I get liver tests while taking azilsartan?
Not routinely - unless you have existing liver disease, drink alcohol regularly, or take other medications that affect the liver. Your doctor may order a baseline test before starting and check again in 3-6 months. After that, annual tests are usually enough.
What’s the safest ARB for someone with liver problems?
Azilsartan and valsartan are among the safest. Both have minimal liver metabolism. Telmisartan and losartan are metabolized more by the liver, so they carry slightly more risk in advanced liver disease. Always discuss alternatives with your doctor.
Can I drink alcohol while taking azilsartan?
Moderate alcohol (one drink a day for women, two for men) is usually fine. But heavy drinking increases liver stress and can raise blood pressure - the exact problem azilsartan is meant to fix. If you have liver disease, avoid alcohol entirely.
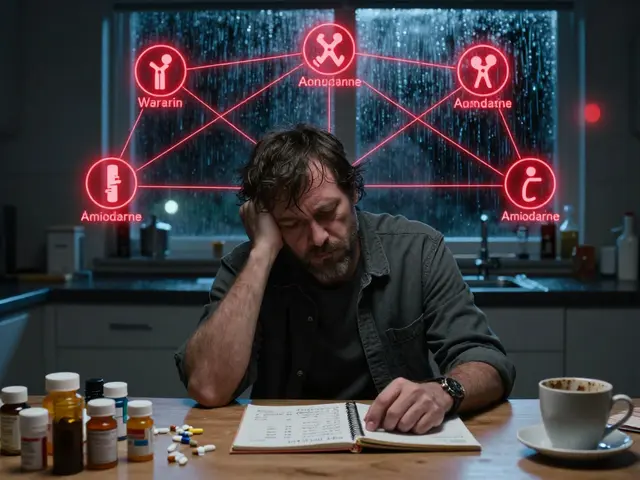
Does azilsartan interact with other liver-metabolized drugs?
Not significantly. Because azilsartan isn’t processed by the main liver enzyme systems (like CYP3A4 or CYP2C9), it rarely interferes with statins, antidepressants, or other common medications. Still, always tell your doctor about every pill or supplement you take.
Next steps if you’re on azilsartan
If you’re taking azilsartan and feel fine - keep going. Don’t change anything unless your doctor says so. If you’re unsure about your liver health, ask for a simple blood test. It takes five minutes and gives you peace of mind.
And if you’re just starting azilsartan? Don’t overthink it. Your liver doesn’t need to be perfect for this drug to work. But staying aware - and staying in touch with your doctor - is how you stay safe, not just healthy.










Camille Mavibas
29 Oct 2025 at 12:33I’ve been on azilsartan for 2 years and my liver enzymes have never budged 😌 I used to panic every time I got blood work done, but now I just smile and say ‘thanks, azil!’ 🙏