When your thyroid goes into overdrive, it doesn’t just make you feel anxious or jittery-it can send your heart racing, your hands shaking, and your body overheating. Hyperthyroidism, or an overactive thyroid, happens when your thyroid gland pumps out too much T3 and T4 hormone. This isn’t just a case of feeling "wired"-it’s a real medical condition that affects about 1.2% of adults in the U.S., and women are far more likely to get it than men. Left unchecked, it can lead to serious heart problems, bone loss, or even a life-threatening crisis called thyroid storm. The good news? You don’t have to wait weeks for treatment to kick in. beta-blockers are the fast-acting tool doctors use to bring your symptoms under control while the real fix takes time.
What’s Really Going On in Your Body?
Your thyroid is a small butterfly-shaped gland in your neck. It’s supposed to produce just enough thyroid hormone to keep your metabolism running smoothly. But when something goes wrong-like Graves’ disease (which causes 60-80% of cases)-your immune system accidentally tells your thyroid to overproduce. Other causes include toxic nodules or inflammation. The result? Your body burns energy too fast. You might sweat through your clothes in a cool room, lose weight even when eating more, feel your heart pounding at rest, or have trouble sleeping because your mind won’t shut off.Why Beta-Blockers? They Don’t Fix the Cause-but They Fix How You Feel
Here’s the key thing to understand: beta-blockers don’t lower your thyroid hormone levels. They don’t stop your thyroid from making too much. That’s the job of antithyroid drugs like methimazole or radioactive iodine therapy. But while those treatments take 3 to 6 weeks to start working, beta-blockers can calm your racing heart and shaky hands in just a few hours. That’s why doctors reach for them right away. If you’re walking into the clinic with a heart rate of 120 beats per minute, trembling hands, and panic attacks, you need relief now. Beta-blockers block the effects of adrenaline on your body. They slow your heart, reduce tremors, ease anxiety, and even help with heat intolerance. In emergency cases like thyroid storm, intravenous esmolol can be given in the ICU to rapidly bring down dangerously high heart rates.Which Beta-Blockers Work Best-and Why Propranolol Is the Go-To
Not all beta-blockers are created equal when it comes to hyperthyroidism. The American Thyroid Association recommends propranolol as the first choice. Why? Because it’s non-selective. That means it blocks both beta-1 and beta-2 receptors. Blocking beta-1 helps with heart rate and tremors. But propranolol also has a special trick: at higher doses, it partially blocks the conversion of T4 (the main hormone your thyroid makes) into T3 (the more active form). That’s a bonus effect no other beta-blocker offers. Typical starting doses are 10-20 mg every 6 hours. Many people need 40 mg three or four times a day. In severe cases, doses can go up to 240-480 mg daily. It’s not unusual for someone with uncontrolled hyperthyroidism to need higher doses than what’s typically prescribed for high blood pressure. Other options include nadolol (taken once daily) and atenolol (a selective beta-1 blocker, sometimes used if you have asthma). But propranolol remains the gold standard because of its dual action and proven track record.
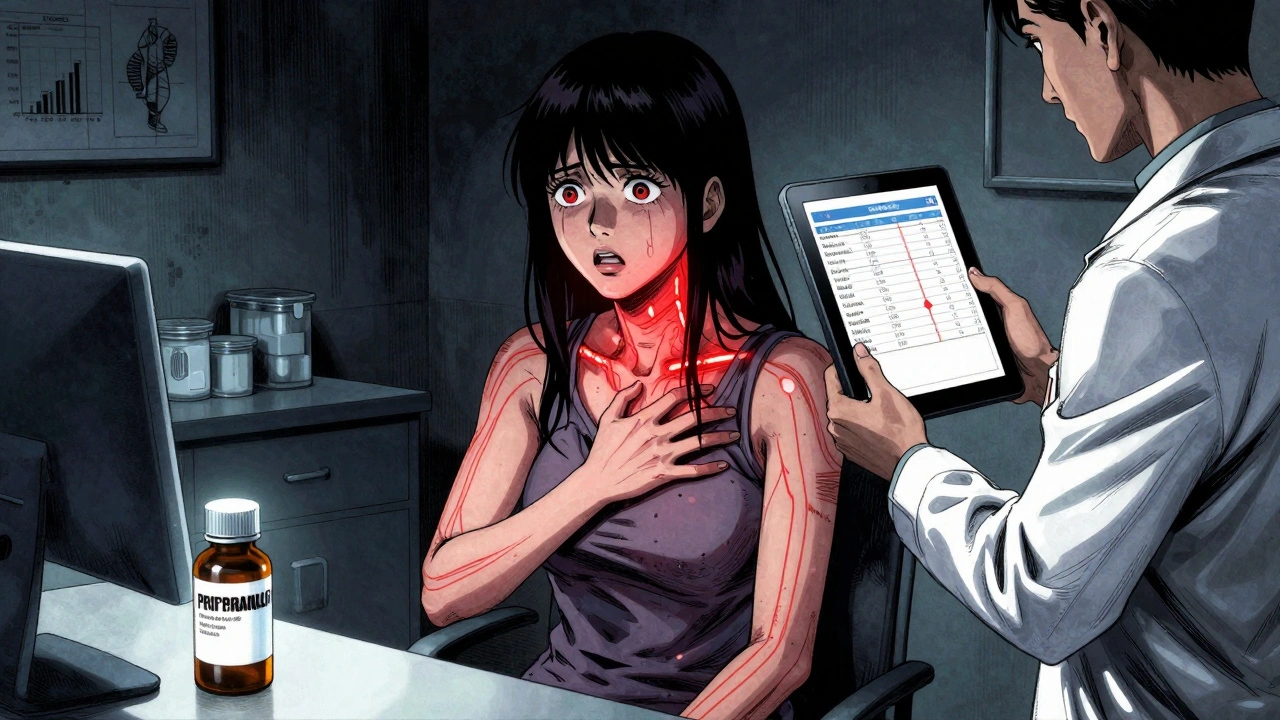
When Beta-Blockers Aren’t Safe-Alternatives for High-Risk Patients
If you have asthma, COPD, or severe heart failure, beta-blockers can be risky. Blocking beta-2 receptors in your lungs can trigger bronchospasm. That’s why the European Thyroid Association recommends calcium channel blockers like verapamil or diltiazem as alternatives. These drugs lower heart rate without affecting your airways. They’re not as effective at reducing tremors or anxiety, but they’re much safer for people with lung conditions. Elderly patients also need careful dosing. Their hearts are more sensitive, and they’re more likely to have other conditions like low blood pressure. Starting with low doses and increasing slowly is critical. Monitoring heart rate and blood pressure regularly is non-negotiable.How Long Do You Stay on Beta-Blockers?
This is where people get confused. Beta-blockers aren’t a cure. They’re a bridge. Once your antithyroid medication starts working and your thyroid hormone levels return to normal (usually within 4-8 weeks), your doctor will start tapering the beta-blocker. You don’t need to stay on them forever. But there’s an exception: if you’re getting radioactive iodine treatment. After RAI, your thyroid can still release stored hormone for weeks or months. During that time, your symptoms might linger. That’s why doctors advise continuing beta-blockers until your thyroid function tests are stable-even if that takes 3 to 6 months. Stopping too early can mean your heart races again, your anxiety spikes, or you end up back in the ER. Waiting until you’re truly euthyroid is the rule.What Happens If You Skip Beta-Blockers?
Some people think, "I’ll just wait for the antithyroid drugs to work." But waiting 4 weeks with a heart rate of 130+ isn’t safe. High heart rates over time can lead to atrial fibrillation, heart failure, or even stroke. A 2021 study showed that patients who started beta-blockers within 24 hours of diagnosis had 37% fewer emergency visits for thyrotoxic symptoms than those who waited. That’s not just comfort-it’s prevention. Skipping beta-blockers also means more time spent feeling miserable. Imagine trying to work, sleep, or care for your kids when your body feels like it’s in overdrive. Beta-blockers don’t just prevent complications-they restore your quality of life while you wait for the real treatment to take effect.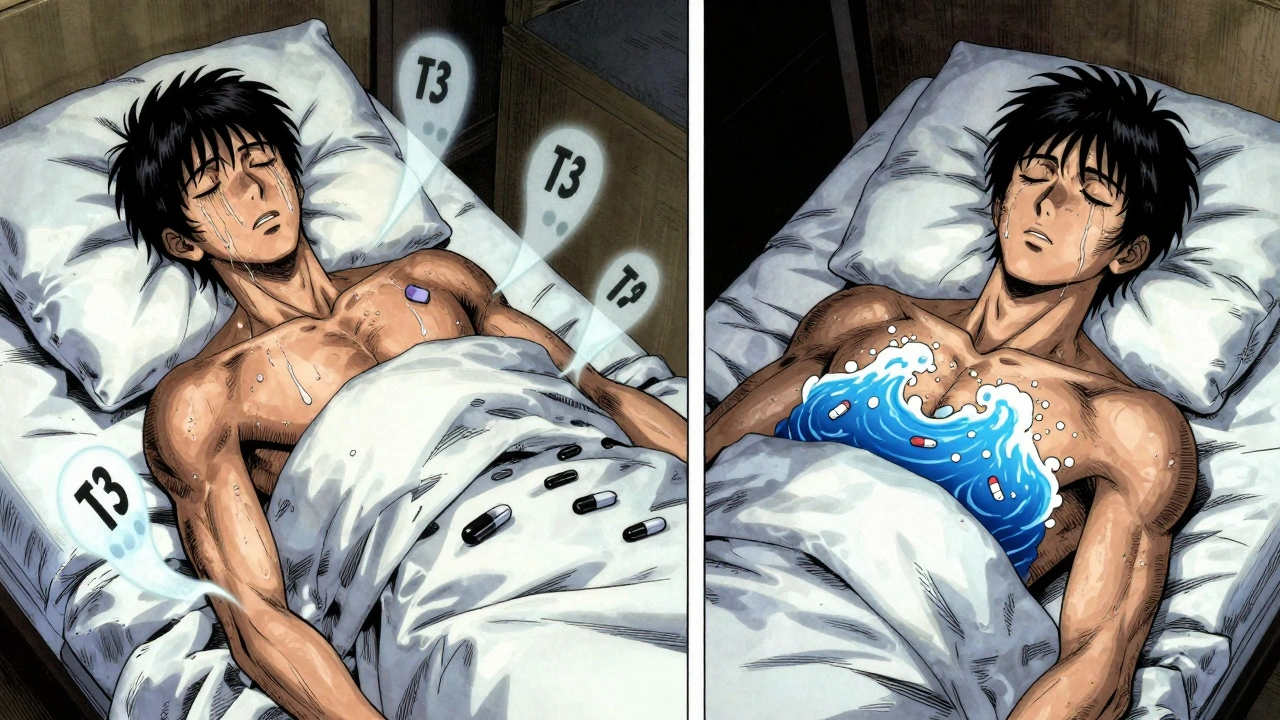
Monitoring and What to Watch For
Your doctor will check your thyroid levels at 6 weeks, then every 3 months until stable. But you also need to monitor your symptoms and vital signs. Keep track of your resting heart rate. If it drops below 50-55 and you feel dizzy or tired, talk to your doctor. That’s a sign you might be on too high a dose. Also, don’t stop beta-blockers suddenly. Abruptly stopping can cause rebound tachycardia or worsen angina. Always taper under medical supervision.Common Misconceptions
One myth is that beta-blockers are just for anxiety. They’re not. In hyperthyroidism, they’re treating a physical, hormone-driven state-not a psychological one. Another myth is that they’re addictive. They’re not. You don’t develop tolerance, and you don’t need to keep increasing the dose over time. Some people worry about side effects like fatigue or cold hands. These are usually mild and temporary. The benefits far outweigh the risks for most patients.What’s Next for Treatment?
Research is looking at newer beta-blockers with more targeted effects, but no major changes are expected before the next ATA guidelines update in 2026. For now, the 2016 recommendations still hold strong. Beta-blockers remain the fastest, safest, and most effective way to manage symptoms while you wait for your thyroid to settle down.Can beta-blockers cure hyperthyroidism?
No. Beta-blockers only manage symptoms like rapid heartbeat, tremors, and anxiety. They don’t reduce thyroid hormone production. Definitive treatment requires antithyroid drugs, radioactive iodine, or surgery.
How quickly do beta-blockers work for hyperthyroidism?
Most people notice improvement in heart rate and tremors within 1-2 hours after taking propranolol. Full symptom control usually happens within a day or two.
Is propranolol the only beta-blocker that works?
No, but it’s the most effective. Propranolol is preferred because it also blocks the conversion of T4 to T3. Other options like nadolol or atenolol work for heart rate and anxiety but lack this extra benefit.
Can I take beta-blockers if I have asthma?
Non-selective beta-blockers like propranolol can worsen asthma. If you have asthma or COPD, your doctor may choose a calcium channel blocker like verapamil or diltiazem instead. Atenolol may be used cautiously in some cases.
How long should I stay on beta-blockers after starting antithyroid medication?
Typically 4-8 weeks, or until your thyroid hormone levels return to normal. If you’re getting radioactive iodine, you may need them for 3-6 months until your thyroid function stabilizes.
Are beta-blockers safe for older adults?
Yes, but with caution. Older adults are more sensitive to heart rate slowing. Doctors start with lower doses and monitor closely for dizziness, low blood pressure, or fatigue.
Can beta-blockers cause weight gain?
Not directly. Weight gain in hyperthyroidism usually happens after treatment starts because your metabolism slows back to normal. Beta-blockers themselves aren’t known to cause weight gain.









Lynn Steiner
3 Dec 2025 at 04:19Ugh, I hate how doctors just throw beta-blockers at you like it’s a magic pill. My cousin took them and became a zombie-no energy, no joy, just numb. Like, yeah, your heart’s racing, but maybe you just need to chill the hell out and stop eating gluten? 😒