When someone overdoses, every second counts. But calling 911 isn’t always the right first step-and not calling it when you should can be deadly. The difference between calling Poison Control and calling emergency services isn’t about being cautious or dramatic. It’s about matching the right response to the real risk. Knowing when to call each one can save a life, avoid an unnecessary ER trip, and keep emergency resources available for those who need them most.
Call 911 Immediately If There Are Life-Threatening Symptoms
If the person is unconscious, not breathing, having seizures, or their heart is racing or crashing, don’t hesitate. Call 911 right away. These aren’t signs you can wait out. They’re red flags that the body is shutting down.The CDC tracks fatal poisonings and finds that 28.3% of deaths involve respiratory failure. That means the person stops breathing-or can’t get enough air. If they’re gasping, turning blue, or unresponsive even when you shake them hard, that’s not a call for advice. That’s a code blue.
Seizures lasting more than five minutes are another emergency. So is a systolic blood pressure below 90 mmHg. That’s dangerously low. It means the heart can’t push blood to the brain or organs. Even if the person was fine five minutes ago, a sudden drop like this can mean internal collapse.
Infants under one year and adults over 79 are especially vulnerable. Their bodies process drugs differently. A dose that might just make an adult drowsy can stop a baby’s breathing or trigger a stroke in an elderly person. If someone in one of these age groups has taken anything unusual-even a single pill-call 911. Don’t wait for symptoms. The risk is too high.
Call Poison Control When the Person Is Stable and You Have Details
If the person is awake, breathing normally, and acting like themselves-or at least not acting dangerously-Poison Control is your best first move. This service isn’t just a hotline. It’s a team of pharmacists and toxicologists trained to handle thousands of cases every day.Most calls to Poison Control are for accidental overdoses. A kid grabs a bottle of vitamins. An older adult takes two pills instead of one. A teenager misreads the label on a sleep aid. These are common. And in most cases, they’re not emergencies. Poison Control can tell you whether to watch, when to go to the ER, or if it’s safe to stay home.
They can also help with timing. Many drugs don’t cause symptoms right away. Acetaminophen, for example, can look harmless for hours-but liver damage starts building. Poison Control uses tools like the Rumack-Matthew nomogram to calculate risk based on how much was taken and when. If someone took less than 150 mg/kg of acetaminophen and is still feeling fine after four hours, they can often be monitored at home with follow-up.
But here’s the catch: you need details. Don’t guess. Don’t say “a bunch of pills.” Say “three 500 mg Tylenol tablets, taken at 3:15 p.m.” Have the bottle ready. Check the label. Is it immediate-release or extended-release? That changes everything. Extended-release pills can keep releasing poison into the body for 12 hours or more.
Know What Information to Have Ready
Whether you’re calling Poison Control or waiting for 911, having the right facts speeds up help. The more accurate your info, the better the advice.- Exact product name and concentration: “Ibuprofen” isn’t enough. Is it Advil? Motrin? 200 mg or 400 mg per tablet? The concentration matters.
- Amount ingested: Count pills. Measure liquids in milliliters. Don’t say “a lot.” Say “two tablespoons of liquid cough syrup.”
- Time of exposure: When did they take it? Within the last 15 minutes? Two hours ago? Timing determines treatment options.
- Patient’s weight: Poison Control calculates doses per kilogram. If you don’t know the weight, estimate as best you can-but know that errors here can lead to wrong advice. A 20-pound child and a 200-pound adult need completely different responses.
- Current symptoms: Are they sleepy? Nauseous? Confused? When did it start? Even small changes matter.
- First aid given: Did you give them milk? Water? Make them throw up? Don’t assume it’s helpful. Some toxins get worse with vomiting.
Keep the bottle or container nearby. The label has formulation details, expiration dates, and warnings that emergency responders might not know. A pill that looks like Tylenol could be a counterfeit with dangerous fillers. Poison Control can cross-reference the product with national databases.

Special Cases That Always Require 911
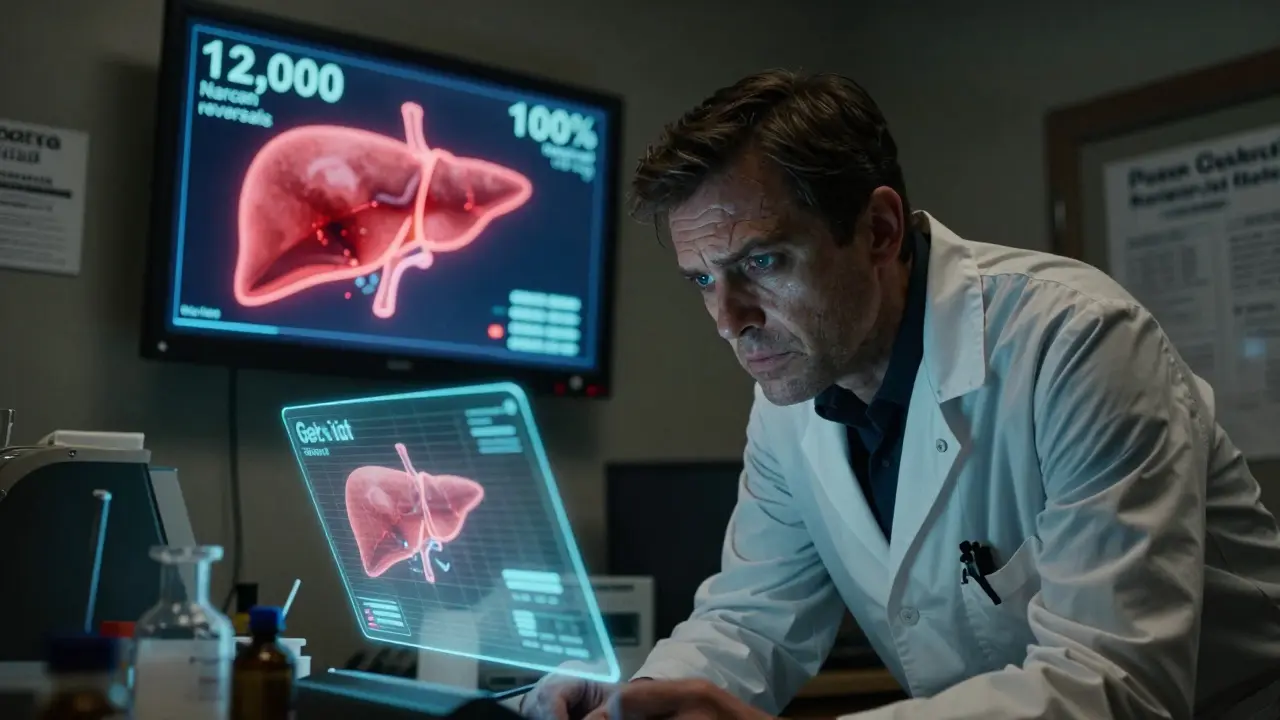
Some situations are never okay to handle over the phone. If any of these apply, call 911 immediately-even if the person seems fine right now.- Opioid overdose: Fentanyl, heroin, oxycodone. Even if you give naloxone (Narcan) and they wake up, call 911. Synthetic opioids like fentanyl can re-sedate someone after naloxone wears off. The New Mexico Health Department reversed over 12,000 overdoses with Narcan in 2022-but every single case required a follow-up 911 call.
- Multiple substances: Mixing alcohol with pills, antidepressants with painkillers, or street drugs with prescription meds creates unpredictable reactions. Over 68% of suicide attempts involve more than one substance. These are high-risk.
- Carbon monoxide exposure: No matter how mild the symptoms-headache, dizziness, nausea-call 911. Carbon monoxide poisoning can cause brain damage hours later, even if the person feels better. There are no safe home treatments.
- High-risk medications: Clonidine (used for ADHD and high blood pressure), sulfonylureas (diabetes drugs), calcium channel blockers, and beta-blockers can cause delayed heart or brain failure. Emergency physicians report that 38% of ER visits for calcium channel blocker overdoses came after people waited too long to call for help.
- Intentional overdose: Whether it’s a suicide attempt or a cry for help, don’t assume someone will be okay. People who intentionally overdose often take more than they admit. Their condition can worsen fast. Call 911.
What Not to Do
There are common myths that cost lives. Don’t do any of these:- Don’t induce vomiting. Ipecac is no longer recommended. It can cause more harm than good, especially with caustic substances or petroleum products.
- Don’t give milk or charcoal unless told to. Activated charcoal works for some toxins-but only if given within an hour and only if the substance is known to bind to it. Giving it randomly can interfere with later treatments.
- Don’t wait to see if they get worse. Some poisons don’t show symptoms for hours. Waiting can turn a treatable case into a fatal one.
- Don’t rely on apps or websites alone. The Poison Help app gives general advice, but it can’t replace a live toxicologist. Over 18% of users misused it for high-risk cases, thinking the app was enough.
Technology Helps, But Doesn’t Replace Expert Advice
There’s a new online tool called webPOISONCONTROL. It’s a free, secure website that walks you through a 12-step questionnaire and gives you a risk level and next steps. In 2022, it handled nearly 30% of all Poison Control consultations. It’s accurate-97% of its recommendations matched what doctors would have said.But it has limits. You can’t use it if the person is already sick. You can’t use it for multiple substances. You can’t use it for children under one year. And you can’t use it if you’re unsure what was taken.
It’s a great tool for quick triage when you’re calm and have all the facts. But if you’re panicking, if the person is changing, or if you’re missing details-call the real people. The Poison Help hotline (1-800-222-1222) connects you to a specialist in under 30 seconds, 24/7.
What Happens After You Call?
If you call Poison Control, they’ll ask questions, assess the risk, and tell you what to do next. In many cases, they’ll say: “Watch for these symptoms. Call back if they appear. No need to go to the ER.” And you’ll feel relieved.But if you call 911, paramedics will come. They’ll check vitals, give oxygen, administer naloxone if needed, and transport to the nearest ER. Emergency rooms are equipped to handle overdoses with IV fluids, antidotes, breathing support, and monitoring.
And here’s the good news: using Poison Control correctly saves money and saves lives. One study found that calling Poison Control instead of going straight to the ER prevented 300,000 unnecessary ambulance rides and hospital visits each year-saving the system $1.8 billion.
But that only works if you call the right service at the right time.
Final Rule: When in Doubt, Call 911
You won’t be wasting anyone’s time. Emergency services are used to this. They’d rather respond to a false alarm than miss a real emergency.And if you’re not sure whether it’s an overdose? Call Poison Control first. They’re trained to tell you if it’s safe to wait-or if you need to dial 911 right away.
There’s no shame in calling. No judgment. No risk of being scolded. Just help.
Can I just use the Poison Help app instead of calling?
The Poison Help app gives general first aid tips and can help you prepare before you call. But it doesn’t connect you to a specialist. If someone is showing symptoms, took multiple substances, or is under 1 or over 79, you need a live expert. The app has helped over a million people-but 18% of users misused it for high-risk cases, thinking it was enough. When in doubt, call 1-800-222-1222.
What if I don’t know what was taken?
Call Poison Control anyway. They can help you identify unknown pills using pictures or descriptions. If you find empty containers, wrappers, or pills nearby, bring them to the phone. Even vague info like “blue round pill” or “clear liquid in a spray bottle” can help. Don’t wait to get all the details-call now.
Is Poison Control free and confidential?
Yes. The Poison Help hotline (1-800-222-1222) is completely free, confidential, and available 24/7. No insurance is needed. No billing. No records kept unless you give permission. It’s funded by the government and hospitals to keep people safe.
Can I call Poison Control for pets?
No. Poison Control handles human exposures only. For pets, call the ASPCA Animal Poison Control Center at (888) 426-4435. There’s a fee for this service, but it’s staffed by veterinary toxicologists who specialize in animal cases. Don’t delay-pets can deteriorate faster than humans.
What if I’m not sure it’s an overdose?
Call anyway. Poison Control specialists are trained to recognize subtle signs of toxicity. Someone might seem fine but be developing internal damage. A child who fell asleep after taking a cough syrup might be in early respiratory depression. A grandparent who feels dizzy after a new blood pressure pill might be having a reaction. It’s better to call and be told it’s nothing than to wait and regret it.
What to Do Next
Save the number: 1-800-222-1222. Put it in your phone contacts as “Poison Control.” Share it with family, caregivers, and babysitters. Post it near the phone or on the fridge.Keep a list of all medications in your home-especially those taken by children or elderly relatives. Store them out of reach. Use childproof caps. Don’t mix pills in unlabeled containers.
And if you ever need help-don’t wait. Call. Even if you’re scared. Even if you think you’re overreacting. You’re not. You’re doing the right thing.










Diksha Srivastava
31 Jan 2026 at 23:39Just saved this post to my phone. My mom takes like 12 different pills and I always panic when she says she feels weird. Now I know when to call Poison Control vs 911. No more guessing. Thank you for making this so clear.
Also, shared it with my aunt who babysits my cousins. Kids find everything, man.