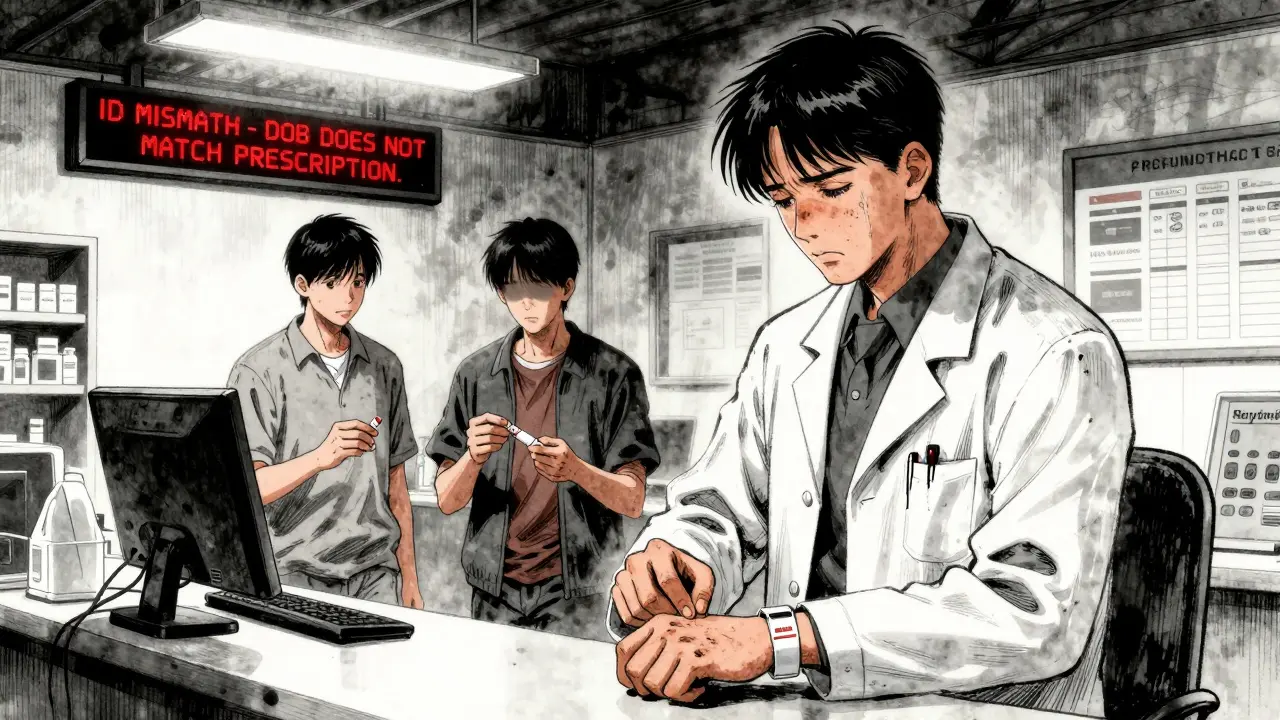
Every year, thousands of patients in the U.S. receive the wrong medication-not because of a mistake in the prescription, but because the pharmacist mixed up who the patient was. It sounds unbelievable, but it happens. And the fix? Simple, but often ignored: using two patient identifiers before handing out any drug. This isn’t just a best practice. It’s a federal safety rule. And when it’s done right, it stops errors before they start.
Why Two Identifiers? The Real Risk
Think about this: two people walk into the same pharmacy on the same day. Both are named John Smith. Both are 62. Both have high blood pressure. One is taking warfarin. The other is allergic to it. If the pharmacist only checks the name, one of them could get a deadly drug. That’s not hypothetical. It’s documented. In 2023, The Joint Commission reported that patient misidentification led to over 2,000 serious medication errors in U.S. hospitals alone. Many more go unreported. The problem isn’t just names. It’s duplicate records. One patient might have three different medical records because they were seen under their middle name once, their nickname another time, and their legal name a third time. A 2024 Altera Health survey found that hospitals without a unified patient database had a 17% mismatch rate when trying to pull up records. That means nearly 1 in 5 patients couldn’t be correctly identified-just by name and date of birth.The Rule: What Counts as a Valid Identifier
The Joint Commission’s National Patient Safety Goal (NPSG.01.01.01) has been clear since 2003: you need two unique identifiers for every patient, every time. But not all identifiers are equal. Room number? No. Insurance ID? No. Email? Not reliable enough. Only these count:- Full legal name
- Date of birth
- Assigned medical record number
- Phone number (if consistently used in the system)
Manual Verification: The Flawed Default
Most community pharmacies still rely on staff asking patients for their name and DOB. Sounds simple. But it’s broken. A 2023 survey by the American Society of Health-System Pharmacists found that 63% of pharmacists admitted to cutting corners during busy hours. Some just nod along when a patient says, “Yeah, that’s me.” Others don’t write down the verification in the system at all. The Joint Commission’s 2023 audits showed that 37% of non-compliant pharmacies failed to document the two-identifier check-meaning even if they did it, no one could prove it. And here’s the kicker: patients often don’t know their own medical record number. They might not remember their exact birthdate. Or they might be confused, elderly, or in pain. Asking them to confirm their identity isn’t a failsafe. It’s a gamble.
Technology That Actually Works
The biggest jump in safety didn’t come from better training. It came from barcodes. In 2012, a study in the Journal of Patient Safety showed that when pharmacies used barcode scanning to match the patient’s wristband with the medication label, medication errors dropped by 75%. Why? Because the system doesn’t ask. It checks. The pharmacist scans the patient’s wristband. The system checks the name, DOB, and medical record number against the prescription. If it doesn’t match, it stops. No debate. No guesswork. Even better? Biometric systems. Imprivata’s palm-vein scanners, used in some hospitals, identify patients with 94% accuracy. That’s a huge leap from the 17% match rate seen in systems without a master patient index (EMPI). These systems don’t rely on memory or cooperation. They use the body itself as the ID. And EMPI? It’s the silent hero. An Enterprise Master Patient Index ties every record-across ER, pharmacy, labs, and specialists-into one clean profile. Without it, duplicate records pile up. One patient, five records, zero safety. With it, a pharmacist can see every drug the patient has ever taken, every allergy, every interaction risk-before they even open the bottle.What Doesn’t Work: Double-Checking Without Tech
You’ve probably heard: “Have two pharmacists check the prescription.” Sounds smart. But a 2020 review in BMJ Quality & Safety found no clear evidence that this reduces errors. Why? Because both pharmacists often rely on the same flawed system. If the name on the label is wrong, two people will miss it. If the DOB is typed in wrong, two people will approve it. And if they’re rushing? They’ll just sign off. Technology doesn’t replace human judgment. It supports it. The real safety net isn’t a second person-it’s a second system that forces verification.
Real Stories: When It Failed
In 2023, a patient was brought to a hospital unconscious. The ER staff couldn’t find his record. They created a new one. Days later, they discovered he had a full medical history under his middle name. He was allergic to penicillin. He’d been prescribed it twice in the past year. Both times, the allergy was buried in a separate record. He survived. Others haven’t. A Reddit thread from a community pharmacist in Ohio described a near-miss: a patient came in for a refill of metformin. The system showed a recent prescription for insulin. The pharmacist didn’t cross-check the DOB. The patient had the same name as someone else with type 1 diabetes. The pharmacist almost gave him insulin. He caught it at the last second-because he noticed the wrong birth year on the label. He didn’t scan. He didn’t use two identifiers. He just got lucky.How to Get It Right
Implementing this isn’t about buying expensive tech overnight. It’s about starting with what you have.- Train staff to always ask for two identifiers-never just one.
- Document every check. Write it down. Log it in the system. If it’s not recorded, it didn’t happen.
- Use barcodes if you can. Even basic barcode scanners on the counter can cut errors by half.
- For high-risk meds (like insulin, opioids, anticoagulants), use a timeout. Stop. Verify. Scan. Confirm. Then dispense.
- Push for an EMPI. If your pharmacy is part of a larger health system, demand that patient records are unified. Duplicate records are a safety hazard, not a paperwork issue.
The Bigger Picture
This isn’t just about pharmacies. It’s about the whole system. The 21st Century Cures Act and CMS rules now treat accurate patient identification as the foundation of interoperability. If you can’t match a patient to their record, you can’t share data. If you can’t share data, you can’t prevent drug interactions. If you can’t prevent drug interactions, patients die. The Office of the National Coordinator for Health IT estimates that duplicate records cost large hospitals $40 million a year in wasted time, retesting, and error correction. That’s not just money. It’s lives. And the future? A national patient identifier is being piloted in 2025. It could be the final piece. But until then, the two-identifier rule is the only thing standing between a patient and a deadly mistake.It’s not complicated. It’s not expensive. It’s just necessary. And if you’re working in a pharmacy? You’re the last line of defense. Don’t let it slip.
What are the two patient identifiers required in pharmacy settings?
The two required identifiers must be unique to the patient and directly tied to their official record. Acceptable identifiers include the patient’s full legal name, date of birth, assigned medical record number, or phone number. Room numbers, insurance IDs, or location-based details like clinic names are not acceptable. Both identifiers must be verified against the prescription and documented in the system.
Is asking a patient their name and DOB enough?
No. While asking for name and date of birth is common, it’s not reliable on its own. Patients may misremember their birthdate, use nicknames, or be confused due to illness. The system must also verify these details against the electronic record. Without scanning or matching against a medical record number, you’re relying on memory-not proof.
Why do some pharmacies skip the two-identifier check?
Time pressure is the biggest reason. In busy community pharmacies, pharmacists may feel rushed and skip documentation or skip verifying the medical record number. A 2023 ASHP survey found 63% of pharmacists admitted to occasional non-compliance, especially during peak hours. Some also believe the system is “obvious” and don’t see the need-but that’s when errors happen.
Can barcode scanning really prevent medication errors?
Yes. A 2012 study in the Journal of Patient Safety showed a 75% reduction in medication errors reaching patients after barcode scanning was introduced. The system matches the patient’s wristband, the medication label, and the electronic prescription in real time. If any detail doesn’t match, the system alerts the pharmacist before the drug is dispensed.
What happens if a pharmacy doesn’t follow the two-identifier rule?
Non-compliance can lead to loss of accreditation from The Joint Commission, which affects Medicare and Medicaid reimbursement. In 2023, it was the third most common violation in hospital surveys. Beyond penalties, it puts patients at risk. One error can lead to hospitalization, permanent injury, or death-and that’s not just a statistic-it’s a family’s reality.







Marie Mee
15 Dec 2025 at 19:12they're watching us through the pharmacy computers i know it i saw the guy in the back room with the red light blinking he's logging everything even my grandma's blood pressure they're selling this info to big pharma so they can make more pills for people who don't even need them