Pneumocystis jirovecii: What It Is, Who It Affects, and How It’s Treated
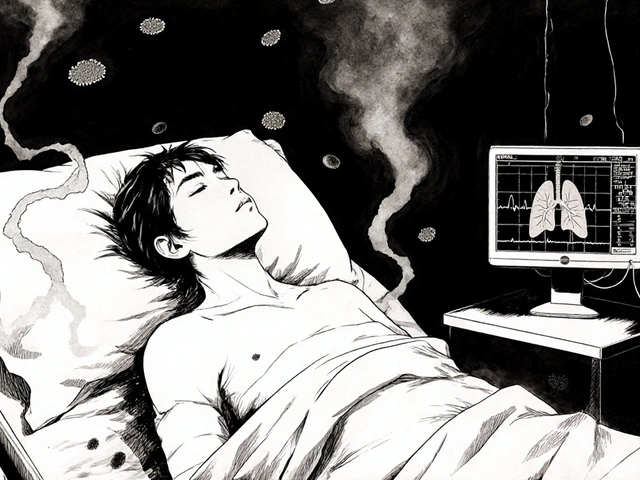
When your immune system is weakened, a tiny fungus called Pneumocystis jirovecii, a fungus that causes pneumonia in people with compromised immune systems. Also known as Pneumocystis carinii, it’s not something you catch from a sneeze—it’s already in your lungs, quietly waiting until your defenses drop. This isn’t a common cold. It’s Pneumocystis jirovecii pneumonia, or PCP, and it’s one of the most dangerous infections for people with HIV, cancer, or those on long-term immunosuppressants.
People on drugs like mycophenolate mofetil, an immunosuppressant used after organ transplants and for autoimmune diseases, or rituximab, a drug that wipes out key immune cells to treat lymphoma or rheumatoid arthritis, are at high risk. Even people taking high-dose steroids for asthma or lupus can slip into danger. PCP doesn’t hit everyone the same way. Some feel like they have the flu—low fever, dry cough, shortness of breath. Others crash fast, needing oxygen or a ventilator. The scary part? It’s treatable, but only if caught early.
Doctors don’t just guess. They test lung fluid or use blood markers to confirm it’s Pneumocystis jirovecii and not a virus or bacteria. The go-to treatment? Trimethoprim-sulfamethoxazole, a combo antibiotic that’s cheap, effective, and has been used for decades. But if you’re allergic, alternatives like pentamidine or atovaquone exist. Prevention is just as important. If you’re on immunosuppressants, your doctor might put you on a daily low-dose antibiotic just to keep this fungus from waking up.
What you’ll find in the posts below aren’t just medical summaries—they’re real-world stories and practical guides from people who’ve faced this. You’ll see how PCP connects to drug interactions, why vaccine timing matters for those on immunosuppressants, and how to spot early signs before it turns critical. This isn’t theory. It’s what happens when a quiet fungus meets a weakened body—and how to stop it before it’s too late.
Immunosuppressed patients face rare, dangerous infections from organisms that rarely affect healthy people. These infections often show no symptoms until it's too late. Understanding the risks and early testing is critical for survival.