More than half of adults over 65 struggle with sleep. They toss and turn, wake up too early, or lie awake for hours. It’s not just annoyance-it’s a health risk. Poor sleep in seniors is linked to falls, memory problems, depression, and even faster cognitive decline. Many reach for a pill: Ambien, Lunesta, Valium, or even melatonin from the drugstore. But what if the fix is worse than the problem?
Why Sleep Pills Are Riskier for Seniors
Your body changes as you age. Liver and kidney function slow down. That means drugs stick around longer. A pill that clears your system in 4 hours when you’re 30 might linger for 12 hours at 70. That’s why a standard dose of zolpidem (Ambien) can leave you groggy, dizzy, and unsteady the next morning-exactly when you’re most likely to get up for the bathroom or walk to the kitchen. The American Geriatrics Society has been warning doctors since 1991: avoid benzodiazepines and Z-drugs as first-line sleep treatments for older adults. Why? Because they increase fall risk by up to 50%. A broken hip in someone over 65 can be life-changing-or fatal. A 2014 study in the BMJ found long-term benzodiazepine use raised Alzheimer’s risk by 51%. Even worse, those who took long-acting versions for over six months saw an 84% higher chance of developing dementia. And it’s not just prescription drugs. Over-the-counter sleep aids often contain diphenhydramine (Benadryl) or doxylamine. These are anticholinergics-chemicals that block acetylcholine, a brain chemical vital for memory and focus. Studies show regular use of these meds is tied to brain shrinkage and higher dementia risk. Yet, they’re still sold as “gentle” sleep helpers.The Drugs to Avoid (and Why)
The 2019 Beers Criteria lists 10 sleep medications as potentially inappropriate for seniors. Here are the biggest concerns:- Benzodiazepines (like diazepam, lorazepam, flurazepam): Long half-lives, cause confusion, increase fall risk, lead to dependence. Flurazepam can stay in your system for days.
- Triazolam (Halcion): Even though it’s short-acting, it’s especially dangerous in older adults. Linked to memory loss, hallucinations, and next-day impairment.
- Z-drugs (zolpidem, eszopiclone, zaleplon): Marketed as safer, but still raise fall risk by 30% in seniors. The FDA added black box warnings in 2020 for complex sleep behaviors-like sleepwalking or driving while asleep.
- Trazodone: Often prescribed off-label as a sleep aid, but it’s an antidepressant. Can cause dizziness, low blood pressure, and urinary retention. Nursing home staff report increased nighttime wandering in residents on this drug.
These aren’t hypothetical risks. On Reddit’s r/geriatrics, dozens of families share stories: “Mom fell after taking Ambien,” “Dad started seeing people who weren’t there,” “Grandma forgot how to use the remote.” The side effects aren’t rare-they’re predictable.
The Safer Alternatives That Actually Work
There are better options. Not because they’re new, but because they’re targeted, low-risk, and backed by science. Low-dose doxepin (Silenor) is one of the safest. At just 3-6 mg daily, it helps you stay asleep without the next-day fog. A 2010 study showed it improved total sleep time by nearly 30 minutes with side effects nearly identical to placebo. Unlike other meds, it doesn’t affect memory or balance. The catch? It’s expensive-around $400 a month without insurance. Ramelteon (Rozerem) works differently. Instead of sedating your brain, it targets melatonin receptors to reset your internal clock. It’s ideal for seniors who have trouble falling asleep but not staying asleep. It reduces sleep latency by about 14 minutes and has zero risk of dependence or next-day impairment. No black box warnings. No fall risk spike. Lemborexant (Dayvigo) is the newest option. Approved in 2020, it blocks orexin-brain chemicals that keep you awake. A 2021 JAMA study found it caused less postural instability than zolpidem in adults over 55. It’s also less likely to cause memory issues. But like doxepin, cost is a barrier: around $500/month. Melatonin (2-5 mg) isn’t a magic bullet, but it’s low-risk. For seniors with circadian rhythm disorders-common after retirement or reduced daylight exposure-it can help shift sleep timing. Don’t expect it to make you pass out. But it can gently nudge your body into sleep mode.
The Real Game-Changer: CBT-I
The American Academy of Sleep Medicine says it clearly: cognitive behavioral therapy for insomnia (CBT-I) is the first-line treatment for older adults. Not a pill. Not a supplement. Therapy. CBT-I isn’t about counting sheep. It’s a structured 6-8 week program that teaches you how to break the cycle of poor sleep. Sessions cover:- Sleep restriction: Limiting time in bed to match actual sleep time, building sleep pressure.
- Stimulus control: Only using bed for sleep and sex-not reading, watching TV, or worrying.
- Cognitive restructuring: Challenging beliefs like “I need 8 hours or I’ll die” or “If I don’t sleep tonight, tomorrow will be ruined.”
- Sleep hygiene: Reducing caffeine after noon, avoiding screens before bed, keeping a cool, dark room.
A 2019 JAMA study found telehealth CBT-I helped 57% of seniors with chronic insomnia achieve remission-with 89% sticking with it. That’s better than most drugs. One 72-year-old woman in Melbourne told her sleep specialist, “After six weeks, I stopped Lunesta. I sleep better now than I have in 20 years.”
And it’s getting more accessible. Digital platforms like Sleepio now offer FDA-cleared CBT-I apps. A 2023 JAMA Neurology study showed they worked just as well as in-person therapy for seniors.
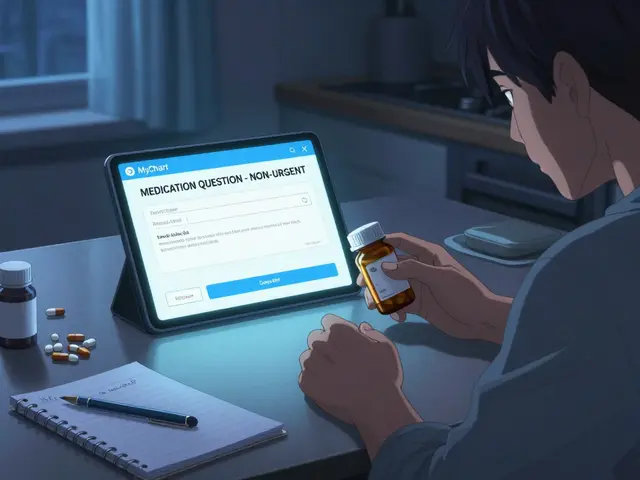
When Medication Is Still Needed
Sometimes, CBT-I isn’t enough. Maybe the person is too ill, too anxious, or too far along in dementia to engage in therapy. Or maybe they’ve been on a sleep med for years and need to come off safely. If medication is unavoidable, follow these rules:- Start low, go slow. Use the lowest effective dose. For ramelteon, start at 4 mg. For doxepin, 3 mg. For melatonin, 2 mg.
- Use it short-term. No more than 2-4 weeks unless closely monitored. Long-term use = higher risk.
- Never combine with alcohol or opioids. That combo can suppress breathing in seniors.
- Monitor for side effects. Watch for dizziness, confusion, falls, or daytime grogginess. If any appear, stop and call your doctor.
- Deprescribe properly. Don’t quit cold turkey. Benzodiazepines and Z-drugs can cause rebound insomnia or seizures if stopped abruptly. Taper over 4-8 weeks with medical supervision.

What You Can Do Right Now
You don’t need a prescription to start improving sleep. Try these steps today:- Get 20-30 minutes of sunlight in the morning. It resets your circadian rhythm.
- Stop caffeine after 2 p.m. Even decaf has enough to disrupt sleep.
- Keep your bedroom cool (18-20°C), dark, and quiet. Use blackout curtains.
- Establish a wind-down routine: warm bath, light stretching, reading a physical book.
- Get up at the same time every day-even on weekends. Consistency matters more than total hours.
- If you’re awake for more than 20 minutes, get out of bed. Go sit in another room with dim light. Don’t check your phone. Return to bed only when sleepy.
These aren’t just tips. They’re evidence-backed strategies that work better than most pills.
Final Thoughts: Sleep Is Not a Problem to Be Medicated
Sleep isn’t broken in seniors. It’s often out of sync. The body’s natural rhythms change. Life gets quieter. Activity drops. The brain gets less light, less movement, less structure. Pills don’t fix that. They mask it. And they come with hidden costs-falls, memory loss, dependence, even dementia. The path to better sleep isn’t through a pharmacy. It’s through routine, light, movement, and patience. CBT-I is the gold standard. Safer meds like doxepin or ramelteon can help in the short term. But the real win? Learning to sleep without a pill.Ask your doctor: “Is this medication really necessary? Have we tried CBT-I first?” If they haven’t mentioned it, ask again. Your sleep-and your safety-deserve more than a quick fix.
Are over-the-counter sleep aids safe for seniors?
No, most are not. Common OTC sleep aids like Benadryl (diphenhydramine) or Unisom (doxylamine) are anticholinergics. These drugs block a brain chemical essential for memory and focus. Long-term use is linked to increased dementia risk and brain shrinkage. Even though they’re sold as “gentle,” they’re among the riskiest sleep aids for older adults. Avoid them unless a doctor specifically approves short-term use.
Can seniors take melatonin safely?
Yes, melatonin is one of the safest options for seniors, especially if the issue is trouble falling asleep due to a misaligned internal clock. Use 2-5 mg about an hour before bed. It doesn’t cause dependence, dizziness, or memory issues. But it won’t make you pass out. It helps your body recognize it’s time to sleep. Avoid high doses-more than 5 mg doesn’t help and may cause grogginess.
What’s the best sleep medication for seniors?
There’s no single “best” drug, but low-dose doxepin (3-6 mg) and ramelteon (8 mg) are the safest options backed by research. Doxepin helps you stay asleep without next-day fog. Ramelteon helps you fall asleep without sedation or dependence. Both have minimal side effects compared to benzodiazepines or Z-drugs. Lemborexant is newer and also safe, but cost is high. Always start with the lowest dose and monitor closely.
How long should seniors take sleep meds?
No longer than 2-4 weeks unless under strict medical supervision. Sleep medications are not meant for long-term use in older adults. Even “safer” drugs like zolpidem or lemborexant carry risks of dependence, falls, and cognitive decline with prolonged use. The goal should always be to use medication as a temporary bridge while building long-term sleep habits through CBT-I and lifestyle changes.
Can I stop my sleep medication cold turkey?
Never. Stopping benzodiazepines or Z-drugs suddenly can cause rebound insomnia, anxiety, seizures, or hallucinations. If you want to stop, work with your doctor to create a tapering plan-usually over 4 to 8 weeks. Reduce the dose slowly, maybe by 10-25% every week. Keep a sleep diary to track progress. If symptoms worsen, pause the taper and consult your doctor.
Is CBT-I really better than pills for seniors?
Yes, and the evidence is clear. CBT-I is the only treatment for insomnia in seniors that’s been proven to work long-term without side effects. A 2019 JAMA study showed 57% of seniors using telehealth CBT-I achieved full remission of insomnia-with 89% sticking with it. That’s better than any drug. Unlike pills, CBT-I teaches skills that last. It doesn’t just help you sleep tonight-it helps you sleep for life.
Why do doctors still prescribe sleep meds to seniors?
Many doctors are unaware of the latest guidelines or feel pressured to offer a quick solution. Sleep complaints are common, and CBT-I isn’t always easy to access. Insurance often doesn’t cover it well. Plus, patients often ask for a pill. But awareness is changing. The FDA, Medicare, and the American Geriatrics Society are pushing back. More doctors are now trained in CBT-I or referring patients to sleep specialists. It’s a slow shift, but it’s happening.
What should I ask my doctor about my sleep medication?
Ask these four questions: 1) Is this drug on the Beers Criteria list for seniors? 2) Have we tried CBT-I first? 3) What’s the lowest dose I can take? 4) How long should I be on this? If your doctor can’t answer these clearly, get a second opinion. Your safety matters more than convenience.









David Chase
30 Dec 2025 at 03:39THIS IS WHY AMERICA IS FALLING APART!!! 🤬 People are taking BENADRYL like candy and then wondering why their grandpa is hallucinating and falling down the stairs!!! The FDA needs to BAN these OTC sleep aids NOW!!! 🚨💊 #WakeUpAmerica