When seniors take pain meds, sleep aids, or anxiety drugs, their bodies don’t process them the same way they did at 40. Slower metabolism, weaker kidneys, and a more porous blood-brain barrier mean even standard doses can push them into dangerous sedation-or worse, overdose. The signs aren’t always obvious. A quiet room, a peaceful nap, a slightly slower breath-these aren’t signs of rest. They could be the early warning of a life-threatening drop in breathing. In fact, over-sedation is one of the most common causes of preventable harm in older adults during medical procedures, at home, or in nursing care. And unlike younger patients, seniors often don’t show the classic signs like loud snoring or flailing limbs. Their symptoms are silent, subtle, and easily missed.
Why Seniors Are at Higher Risk
A 75-year-old taking 5 mg of oxycodone isn’t getting the same effect as a 45-year-old. By age 60, liver function drops by 30-50%. Kidneys clear drugs 0.8 mL per minute slower every year after 40. That means medications stay in the system longer, building up over days. Add in multiple prescriptions-painkillers, anti-anxiety meds, sleep aids-and you’ve got a perfect storm. The American Society of Anesthesiologists found that seniors are 3.5 times more likely to suffer respiratory depression from sedatives than younger adults. And 65% of all opioid-related respiratory arrests in hospitals happen in patients over 65.What to Look For: The Silent Signs of Over-Sedation
Don’t wait for blue lips or unresponsiveness. By then, it’s too late. Watch for these early warning signs:- Slowed breathing-fewer than 8 breaths per minute. This is the biggest red flag.
- Shallow breathing-chest barely rising, breaths too light to hear.
- Confusion or drowsiness-hard to wake, slurred speech, not recognizing family.
- Low oxygen levels-SpO2 below 92%, especially if they’re on oxygen and still dropping.
- Slow heart rate-under 50 beats per minute.
- Unusual quietness-a normally talkative person suddenly silent, even when awake.
Here’s the catch: if a senior is on supplemental oxygen, their pulse oximeter might still read 94% even when they’re barely breathing. That’s called silent hypoxia. The machine says they’re fine. But their lungs aren’t moving air. That’s why you can’t rely on oxygen levels alone.
Monitoring Tools That Actually Work
In hospitals, the gold standard is multimodal monitoring-using more than one device at once. At home, you don’t need fancy gear, but you do need to know what to watch.Capnography: The Most Important Tool
Capnography measures carbon dioxide (CO2) in exhaled breath. It doesn’t care if oxygen is being pumped in. If CO2 levels rise above 45 mmHg or the breathing pattern flattens, it’s a clear sign of dangerous hypoventilation. Studies show capnography catches breathing problems 12-14 minutes before oxygen levels drop. That’s a full 12 minutes to react. In seniors, it’s 92% accurate at detecting apnea-far better than pulse oximetry alone.Pulse Oximetry: Still Useful, But Not Enough
A pulse oximeter measures blood oxygen. Keep it on if you have one. But set the alarm at 90%-not 94%. And never ignore a slow breathing rate just because the number looks okay. If their breaths are shallow and slow, even with 95% SpO2, it’s a problem.Respiratory Rate: Count It Yourself
Watch their chest rise and fall for 30 seconds. Multiply by two. If it’s below 8, call for help. If it’s irregular-long pauses, gasping, then fast breaths-that’s also dangerous. Do this every 15-30 minutes if they’re on sedating meds.Level of Consciousness: Use RASS
The Richmond Agitation-Sedation Scale (RASS) is simple:- +2: Agitated
- +1: Restless
- 0: Calm and alert
- -1: Drowsy but awakens easily
- -2: Sleepy, needs loud voice to wake
- -3: Only wakes with physical shake
- -4: Unresponsive to shake
- -5: Comatose
If they’re at -3 or lower, they’re in moderate to deep sedation. That’s a medical emergency. Don’t wait. Call 911 or get them to a hospital.

What to Do If You Notice Warning Signs
If you see any of these signs:- Stop giving any more sedating medication-no more pain pills, sleep aids, or anxiety drugs.
- Call emergency services immediately. Say: “My elderly parent is showing signs of opioid overdose-slow breathing, unresponsive.”
- Keep them awake. Gently shake their shoulder, talk loudly. Don’t let them sleep.
- Position them on their side. This keeps the airway open.
- If you have naloxone (Narcan), use it. It reverses opioid overdose. Inject or spray into the nose. Wait 2-3 minutes. If no improvement, give a second dose.
Naloxone is safe-even if they’re not overdosing, it won’t hurt them. And it can save their life.
Prevention Starts at Home
The best way to avoid overdose is to prevent it before it starts.- Ask for dose adjustments. Tell the doctor: “My parent is over 70. Can we start with half the usual dose?”
- Use the formula: Standard dose × (1 - 0.005 × (age - 20)). For an 80-year-old, that’s 70% of the normal dose.
- Review all meds monthly. Many seniors take 5-10 drugs. Some interact dangerously. A pharmacist can spot the risks.
- Use one pharmacy. That way, they can flag dangerous combinations.
- Keep naloxone on hand. It’s available without a prescription in most states and Australia. Keep it near the bed.
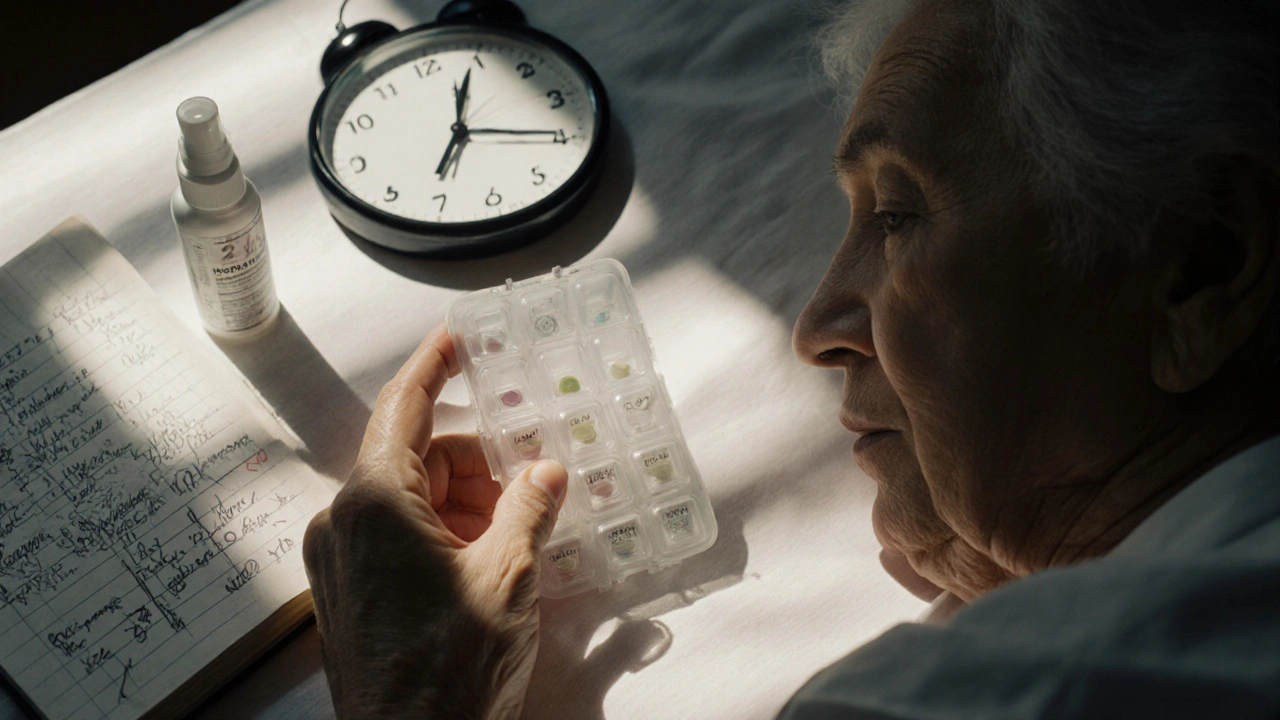
- Use a pill organizer with alarms. Missed doses can lead to rebound pain and overmedication later.
What Facilities Should Be Doing
If your loved one is in a hospital, nursing home, or outpatient clinic, they should be monitored with:- Continuous capnography (not just intermittent checks)
- Pulse oximetry with alarms set at 90%
- ECG to track heart rate
- Non-invasive blood pressure every 5 minutes
- Regular RASS scoring every 15-30 minutes
Only 42% of outpatient endoscopy centers use continuous capnography for seniors. That’s unacceptable. If you’re scheduling a procedure, ask: “Will you use capnography? Will someone be watching breathing continuously?” If they say no, push back. Or go elsewhere.
Common Mistakes That Put Seniors at Risk
- Assuming oxygen masks mean safety. Oxygen can hide low breathing.
- Waiting for obvious signs. By the time they’re unresponsive, it’s too late.
- Using adult doses. 42% of facilities still give seniors the same dose as a 30-year-old.
- Ignoring irregular breathing. Seniors often have uneven breaths. That doesn’t mean it’s normal.
- Over-relying on machines. Alarms go off. Staff get used to them. If they’re not trained to interpret them, they’ll miss the real danger.
Real Stories, Real Consequences
At Mayo Clinic, combining RASS scoring with capnography cut oversedation in patients over 75 by 41%. At Massachusetts General Hospital, a 90-year-old died during a feeding tube procedure because staff only checked oxygen every 10 minutes-and missed 7 minutes of near-zero breathing.One nurse in Melbourne told me about an 82-year-old man on morphine after hip surgery. His oxygen stayed at 95%. But his breathing dropped to 6 per minute. The capnography alarm went off. The nurse intervened before he turned blue. He’s still alive today because they were watching CO2, not just oxygen.
Final Takeaway
Monitoring seniors for over-sedation isn’t about high-tech gadgets. It’s about paying attention. Count breaths. Watch for stillness. Ask: “Is this normal?” If their breathing is slow, shallow, or irregular-don’t wait. Don’t assume they’re just sleeping. Act. Use naloxone if you have it. Call for help. Their life might depend on your quick response.Can seniors overdose on over-the-counter sleep aids?
Yes. Even common sleep aids like diphenhydramine (Benadryl, Sominex) or doxylamine (Unisom) can cause dangerous sedation in seniors. These drugs are anticholinergics, which slow breathing and cause confusion. Doses meant for younger adults can be toxic in people over 65. Always check with a pharmacist before giving any OTC sleep aid to an elderly person.
How often should I check on a senior taking sedatives?
Check every 15-30 minutes during the first 2-4 hours after a dose, then every hour for the next 6-8 hours. If they’re on long-acting opioids or multiple sedating drugs, check every hour for 24 hours. Look for breathing rate, skin color, and responsiveness-not just if they’re asleep.
Is naloxone safe for seniors?
Yes. Naloxone (Narcan) is safe for seniors. It reverses opioid effects but doesn’t harm someone who hasn’t taken opioids. If you’re unsure whether they overdosed, give it anyway. It’s a life-saving tool with no serious side effects in elderly patients. Keep it in your medicine cabinet, like an EpiPen.
What if my senior has COPD? Can I still use capnography?
Yes, but interpretation is trickier. Seniors with COPD often have higher baseline CO2 levels. The key isn’t the absolute number-it’s the trend. A sudden rise in CO2, a flattening waveform, or a drop in respiratory rate over time signals danger, even if numbers seem “normal” for them. Training on COPD-specific waveforms is essential for caregivers and staff.
Can I monitor at home without medical devices?
Yes. You don’t need a machine. Count breaths for 30 seconds every hour. Watch for chest movement. Listen for quiet or shallow breathing. Check if they respond to voice or gentle shake. If they’re unusually sleepy, hard to wake, or breathing fewer than 8 times per minute-call for help immediately. Your eyes and ears are your most important tools.











Joseph Townsend
17 Nov 2025 at 03:10Okay but let’s be real-this isn’t just about meds. It’s about how we treat our elders like broken appliances. You don’t just ‘monitor’ a person like a thermostat. You listen. You sit with them. You notice when their laugh gets quieter. I had my grandma slip into this silent zone after her pain pump kicked in. The nurses said she was ‘resting.’ I said she was dying quietly. They didn’t believe me until her CO2 hit 60. Now I keep Narcan in her sock drawer. Not because I expect it. But because I refuse to be surprised again.
And yeah, capnography? It’s not fancy. It’s just the difference between ‘she’s sleeping’ and ‘she’s gone.’
Stop treating seniors like they’re ghosts. They’re still here. Even when they’re quiet.
Also-why the hell are we still using adult doses? Are we trying to kill them gently?
Also also-Naloxone is cheaper than a pizza. Get it. Now.