Most people don’t talk about hemorrhoids - not because they’re rare, but because they’re embarrassing. But here’s the truth: hemorrhoids affect about 75% of people at some point in their lives. If you’ve ever seen bright red blood on toilet paper, felt a tender lump near your anus, or been too uncomfortable to sit through a meeting, you’re not alone. The real issue isn’t having hemorrhoids - it’s not knowing the difference between internal and external ones, or what actually works to fix them.
What Exactly Are Hemorrhoids?
Hemorrhoids aren’t some weird abnormality. They’re normal blood vessels that help control stool passage. Think of them like little cushions inside your rectum and around your anus. When they get swollen from pressure - from straining during a bowel movement, sitting too long, pregnancy, or chronic constipation - they become problematic. That’s when you feel the itching, pain, or bleeding. The key difference between internal and external hemorrhoids comes down to location - and that determines your symptoms.Internal Hemorrhoids: Silent but Not Harmless
Internal hemorrhoids form inside the rectum, above a line called the dentate line. This area has no pain receptors, so even when they swell, you often won’t feel pain. That’s why many people don’t realize they have them until they see blood. The main sign? Bright red blood on toilet paper, in the toilet bowl, or streaking your stool. It’s usually painless. You might also feel like your bowels aren’t fully empty, or that something’s bulging out. Doctors grade internal hemorrhoids on a scale from I to IV:- Grade I: Bleeds but doesn’t prolapse (protrude).
- Grade II: Prolapses when you strain but pops back in on its own.
- Grade III: Prolapses and needs to be pushed back in by hand.
- Grade IV: Stays outside permanently and can’t be pushed back.
External Hemorrhoids: Painful and Visible
External hemorrhoids form under the skin around the anus - an area packed with nerves. That’s why they hurt. Even a small one can feel like a tender, itchy lump. Sitting becomes a chore. You might notice swelling or a soft skin tag after it shrinks. The worst kind? Thrombosed external hemorrhoids. This happens when a blood clot forms inside the vein. It turns into a hard, purple or blue lump that feels like a bruise. The pain hits fast - often during or right after a bowel movement. It’s sharp, intense, and makes sitting or walking uncomfortable. Unlike internal hemorrhoids, external ones don’t usually bleed unless they rupture. But the pain? That’s unforgettable.Can You Have Both at Once?
Yes. And it’s more common than you think. Many people have a mix - an internal hemorrhoid that’s prolapsed and an external one that’s swollen. This makes symptoms confusing. You might have bleeding from inside, pain from outside, and itching everywhere. That’s why self-diagnosis often fails. That’s also why seeing a doctor matters. Other conditions - like anal fissures, colon polyps, or even colorectal cancer - can mimic hemorrhoid symptoms. Fissures cause a sharp, tearing pain during bowel movements, not the dull ache or itch of hemorrhoids. Cancer doesn’t always cause pain, but it can cause bleeding, changes in bowel habits, or unexplained weight loss. Never assume bleeding is just hemorrhoids. Get it checked.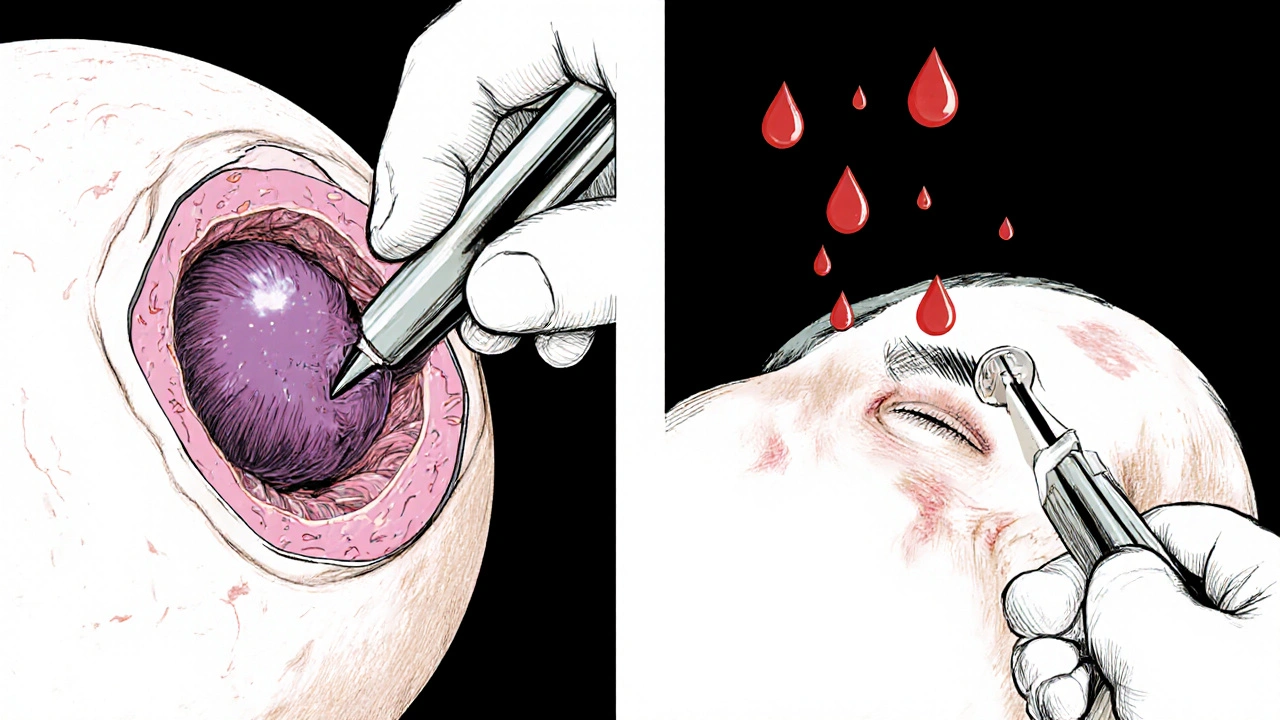
What Causes Hemorrhoids?
It’s not just bad habits. It’s a mix of factors:- Chronic constipation or diarrhea - both make you strain.
- Sitting for long periods, especially on the toilet.
- Pregnancy - the baby’s weight presses on pelvic veins.
- Obesity - extra weight increases pressure in the lower body.
- Heavy lifting - like moving furniture or lifting weights.
- A low-fiber diet - leads to harder stools and more straining.
Treatment: From Home Fixes to Surgery
The good news? Most hemorrhoids get better without surgery - if you act early.Home Care for Mild Cases
Start here:- Eat more fiber: Aim for 25-30 grams daily. Think beans, lentils, oats, apples, pears, broccoli, and whole grains. Most people get less than half that.
- Drink water: At least 8-10 glasses a day. Fiber needs water to work. Without it, you’ll just get bloated.
- Don’t sit on the toilet too long: Limit it to 5 minutes. Use a small footstool to raise your knees above your hips. This position reduces pressure on your rectum by about 30%.
- Take sitz baths: Soak in warm (not hot) water for 15-20 minutes, 2-3 times a day. It reduces swelling and soothes irritation.
- Use over-the-counter creams: Hydrocortisone cream helps with itching. Witch hazel pads reduce inflammation. Avoid products with benzocaine or lidocaine long-term - they can irritate skin.
Minimally Invasive Procedures
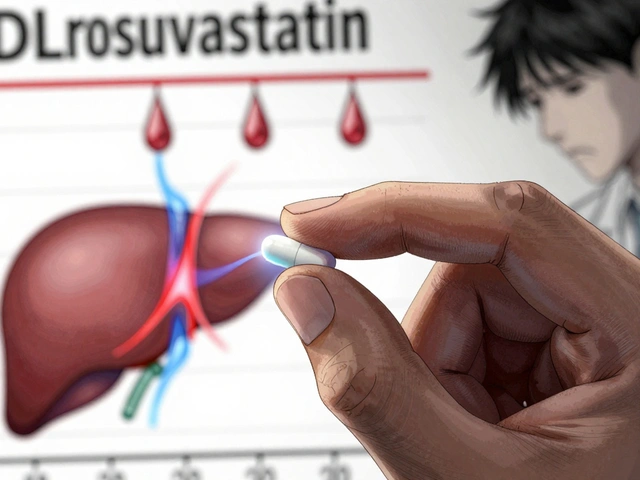
If home care doesn’t help after a couple of weeks, your doctor might suggest one of these:- Rubber band ligation: A tiny rubber band is placed around the base of the internal hemorrhoid. It cuts off blood flow. The hemorrhoid shrinks and falls off in a few days. It’s 90% effective for Grades I-III. You might feel pressure or mild cramping for 1-2 days.
- Sclerotherapy: A chemical solution is injected into the hemorrhoid to shrink it. Less painful than banding, but slightly less effective.
- Infrared coagulation: A brief burst of heat seals the blood vessels. Good for smaller hemorrhoids.
Thrombosed External Hemorrhoids
If you have a painful, purple lump that appeared suddenly, see a doctor within 72 hours. The best fix? A small cut to drain the clot. It’s quick, done under local numbing, and gives almost instant relief. Waiting longer means more pain and slower healing.Surgery for Severe Cases
If hemorrhoids keep coming back or are Grade IV, surgery might be the answer:- Hemorrhoidectomy: The hemorrhoid is completely removed. It’s the most effective option - 95% success rate. But recovery takes 2-4 weeks. Pain is real. You’ll need prescription pain meds for 7-10 days.
- Stapled hemorrhoidopexy: Used mainly for prolapsed internal hemorrhoids. The surgeon staples the tissue back up, cutting off blood flow. Less pain than traditional surgery, but higher chance of recurrence.
What Doesn’t Work
There’s a flood of online products promising “miracle cures” - creams, oils, supplements, teas. Most are useless. Some are harmful. The American Gastroenterological Association warns against them. No pill or potion shrinks hemorrhoids. Only lifestyle changes and proven medical treatments do.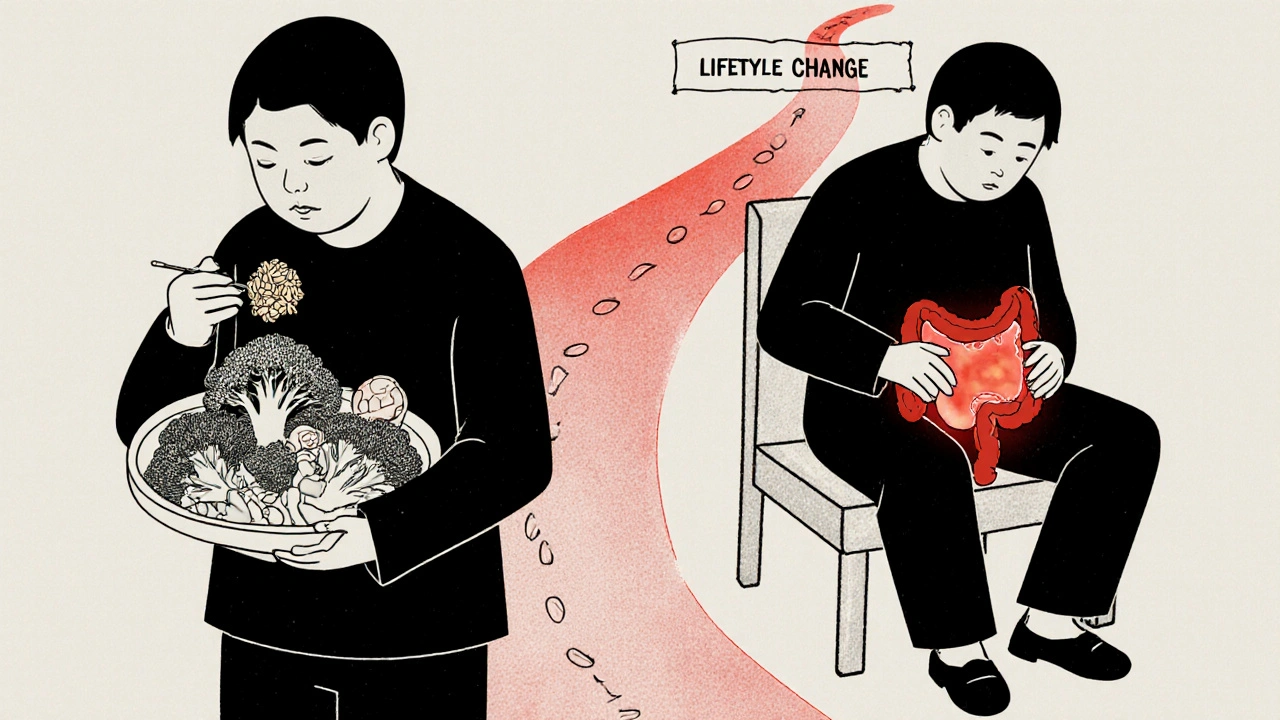
Prevention Is the Real Win
Once you’ve had hemorrhoids, you’re more likely to get them again. But you can cut that risk by 80% if you stick to these habits:- Keep your fiber intake at 30g daily.
- Drink enough water - your urine should be pale yellow.
- Move regularly. Walk 20-30 minutes a day.
- Don’t delay bowel movements. Holding it in increases pressure.
- For pregnant women: sleep on your left side. Do pelvic floor exercises.
When to See a Doctor
Don’t wait until it’s unbearable. Call your doctor if:- Bleeding lasts more than a week or gets worse.
- Pain doesn’t improve after a week of home care.
- You feel dizzy, weak, or light-headed - signs of blood loss.
- Your bowel habits change - constipation, diarrhea, or narrow stools.
- You’re over 45 and haven’t had a colon cancer screening.
Final Thought: You’re Not Alone
Sixty-eight percent of people wait over six months before seeing a doctor for hemorrhoids. Shame keeps them silent. But this isn’t a moral failing. It’s a physical one - and it’s treatable. The sooner you act, the less painful, expensive, and disruptive it becomes. Start with fiber. Drink water. Don’t sit too long. If it doesn’t get better, see a doctor. There’s no shame in asking for help. Your body is trying to tell you something. Listen to it.Can internal hemorrhoids turn into external ones?
No, they don’t transform. Internal and external hemorrhoids form in different areas. But an internal hemorrhoid can prolapse - meaning it pushes out through the anus - and then become mixed with an existing external one. This creates a combined condition that feels like both types at once. It’s not a transformation - it’s a coexistence.
Do hemorrhoids go away on their own?
Mild hemorrhoids often shrink on their own within a few days, especially with home care like sitz baths, fiber, and hydration. But they rarely disappear completely unless the root cause - like constipation or sitting too long - is fixed. Without lifestyle changes, they tend to come back. Think of it like a sprained ankle: rest helps, but if you keep running on it, it never fully heals.
Is it safe to pop a thrombosed hemorrhoid at home?
Never. Trying to pop or cut a thrombosed hemorrhoid yourself risks serious infection, uncontrolled bleeding, or scarring. The clot needs to be drained in a sterile environment by a doctor. It’s a quick, simple procedure under local anesthetic. The pain relief is immediate. Self-treatment can make things much worse.
Can hemorrhoids cause cancer?
No, hemorrhoids themselves do not cause cancer. But rectal bleeding - a common symptom of hemorrhoids - is also a sign of colorectal cancer. That’s why any new or unexplained bleeding, especially after age 45, needs to be evaluated by a doctor. Don’t assume it’s just hemorrhoids. A colonoscopy or rectal exam can rule out more serious conditions.
How long does recovery take after rubber band ligation?
Most people return to normal activities the same day or the next. You might feel mild pressure or cramping for 24-48 hours. The hemorrhoid usually falls off in 5-7 days. Light bleeding or spotting can happen then - that’s normal. Avoid heavy lifting or straining for a week. Full healing takes about two weeks. Follow-up is recommended to check progress.
Are hemorrhoids more common in men or women?
They affect men and women equally overall. But women are more likely to develop them during pregnancy - up to 35% of pregnant women experience them. The added pressure from the growing baby and hormonal changes relax the veins. After childbirth, many improve on their own. Men are more likely to develop them due to heavy lifting or prolonged sitting, especially in desk jobs.
Can diet alone cure hemorrhoids?
Diet alone won’t cure advanced hemorrhoids, but it’s the most powerful tool for preventing them and shrinking mild ones. A high-fiber diet softens stool, reduces straining, and cuts pressure on rectal veins. Studies show people who eat 30g of fiber daily and drink enough water report 80% fewer symptoms. For Grade I or II hemorrhoids, diet and hydration are often enough. For Grade III or IV, medical treatment is needed - but diet still prevents recurrence.
What’s the difference between hemorrhoids and anal fissures?
Both cause bleeding and discomfort, but they’re different. Hemorrhoids are swollen veins - they cause itching, swelling, and dull pain. Fissures are small tears in the anal lining - they cause sharp, tearing pain during bowel movements, often followed by a burning sensation. Fissures rarely cause visible lumps. Bleeding from fissures is usually minimal. Misdiagnosing a fissure as a hemorrhoid leads to ineffective treatment. A doctor can tell the difference with a simple exam.









Josh Gonzales
25 Nov 2025 at 20:53Just want to say fiber and water are the real MVPs here. I used to have flare-ups every month until I started eating lentils for lunch and chugging 3 liters of water a day. No more sitting on the toilet like it’s a second home. Simple. Free. Works.
Also, don’t fall for those ‘miracle hemorrhoid tea’ scams. I bought one. It tasted like dirt and did nothing.