Some medications are like walking a tightrope. One step too far, and things can go wrong - fast. These are called narrow therapeutic index drugs, or NTI drugs. They work great when the dose is just right. But if it’s even a little too high or too low, you could end up in the hospital - or worse. This isn’t theory. It’s real life for hundreds of thousands of people taking these drugs every day.
What Exactly Is a Narrow Therapeutic Index?
Think of your body like a car. Some drugs are like cruise control - they work fine even if you’re a little off. NTI drugs are like a jet engine. If the fuel mix is even slightly wrong, it can stall or explode. The difference between the dose that helps and the dose that harms is tiny - often less than double. For example, with warfarin, your blood needs to clot just enough to prevent a stroke but not so much that you bleed internally. That balance is razor-thin.
The FDA defines NTI drugs as those where small changes in blood levels can cause serious harm: life-threatening reactions, permanent disability, or major complications. That’s why these drugs aren’t treated like regular pills. They need special care - regular blood tests, strict dosing, and sometimes even staying on the same brand.
Common NTI Drugs You Might Be Taking
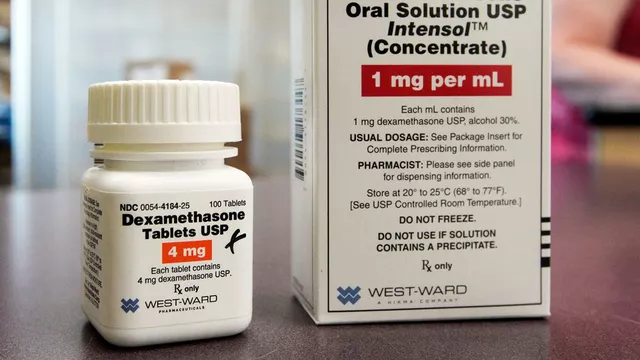
You might not realize you’re on an NTI drug. Here are the most common ones:
- Warfarin (Coumadin, Jantoven): Used to prevent blood clots. Too little? Risk of stroke. Too much? Risk of uncontrolled bleeding. Your INR level must stay between 2.0 and 3.0 for most people.
- Lithium (Lithobid): For bipolar disorder. Therapeutic range? 0.6 to 1.2 mmol/L. Above 1.5? You could start shaking, getting confused, or even have seizures.
- Levothyroxine (Synthroid): For hypothyroidism. Even small changes in dose can make you tired, gain weight, or feel anxious. Many patients report big swings in TSH levels after switching generic brands.
- Digoxin (Lanoxin): For heart failure and irregular heartbeat. Normal level: 0.5 to 0.9 ng/mL. Above 2.0? Life-threatening heart rhythms can start.
- Tacrolimus (Prograf): For transplant patients. Too low? Your body rejects the new organ. Too high? Your kidneys get damaged.
- Phenytoin (Dilantin) and Carbamazepine (Tegretol): For seizures. Tiny changes can trigger seizures or cause dizziness, nausea, or even liver damage.
- Methotrexate (Trexall): Used for cancer, rheumatoid arthritis, and psoriasis. A small overdose can destroy bone marrow and cause severe infections.
These aren’t rare. Millions of people take them. But most don’t know how fragile their balance is.
Why Generic Switches Can Be Dangerous
You’ve probably heard that generics are just as good as brand names. For most drugs, that’s true. But for NTI drugs? Not always.
The FDA allows generics to be 80% to 125% as strong as the brand. That’s a 45% variation - fine for antibiotics or blood pressure pills. But for NTI drugs? That’s a disaster waiting to happen. A 10% change in blood level can push you from safe to toxic.
Real stories prove it. One warfarin patient switched from Coumadin to a generic and saw their INR jump from 2.5 to 4.1 in just one week. That’s a bleeding emergency. Another person switching levothyroxine brands saw their TSH level go from 1.8 to 8.4 - meaning their thyroid was practically shut down. Fatigue, weight gain, depression - all from a pill that looked the same.
That’s why the FDA and EMA now require stricter testing for NTI generics. The acceptable range for bioequivalence has been tightened to 90% to 111% - less than a quarter of the variation allowed for other drugs. Some states, like North Carolina, even require pharmacists to get doctor approval before switching NTI drugs.

What You Must Do to Stay Safe
If you’re on an NTI drug, you’re not just a patient. You’re a manager. Here’s what you need to do:
- Get regular blood tests. Warfarin? INR every 1-4 weeks. Lithium? Every 3-6 months. Tacrolimus? Twice a week at first. Don’t skip them. These tests aren’t paperwork - they’re your safety net.
- Stick with the same brand or generic. If your doctor prescribes Synthroid, ask for it by name. Don’t let the pharmacy swap it unless you’re told it’s safe. Even different generic makers can have different fillers or coatings that change how your body absorbs the drug.
- Know the signs of too much or too little. For warfarin: bruising easily, nosebleeds, dark urine? Too much. Swelling in your leg, chest pain? Too little. For lithium: tremors, nausea, confusion? Too high. Feeling sluggish, cold, gaining weight? Too low. Write these down. Bring them to your doctor.
- Track your meds and symptoms. Use a notebook or a phone app. Note your dose, when you took it, how you felt, and your test results. Patients who do this have 32% fewer bad reactions.
- Watch what you eat and drink. Warfarin reacts with vitamin K - found in leafy greens. One week you eat salads every day, the next you skip them? Your INR will swing. Keep your diet steady. Alcohol, certain antibiotics, and even grapefruit juice can interfere with NTI drugs. Ask your pharmacist what to avoid.
The Bigger Picture: Why This Matters
NTI drugs make up only 5-7% of all prescriptions. But they cause nearly 15% of serious drug-related hospital visits. That’s not because the drugs are bad. It’s because they’re powerful - and easy to mess up.
Hospitals now use barcode scanning on 12 high-risk NTI drugs to prevent dosing errors. Researchers are studying genetic tests to predict how you’ll respond to warfarin or methotrexate. By 2026, genetic testing could be standard before starting these drugs, cutting side effects by up to 35%.
This isn’t just about pills. It’s about control. You’re not helpless. You’re the most important person in your treatment team. Your questions, your notes, your consistency - they save your life.

What to Ask Your Doctor
Don’t be shy. These questions matter:
- Is this drug on the NTI list? Can you show me the name?
- What blood test do I need, and how often?
- Can I stay on the same brand or generic? What happens if I switch?
- What symptoms mean I’m too high or too low?
- Are there any foods, supplements, or other meds I must avoid?
- Is there a tracking app you recommend?
If your doctor doesn’t know the answers, ask for a pharmacist. Pharmacists are NTI experts. They see the risks before you do.
You’re Not Alone
People on NTI drugs often feel anxious. They worry about every pill, every test, every change. But many also find strength in routine. One Reddit user on r/BipolarReddit shared: ‘Regular lithium tests kept me stable for eight years. Before that, I was hospitalized three times in two years.’
You can have that kind of control too. It takes work. But it’s worth it. These drugs aren’t dangerous if you treat them with respect. They’re life-saving - if you know how to use them.
Are all generic drugs unsafe for NTI medications?
No, not all generics are unsafe. But for NTI drugs, even small differences in how the body absorbs the drug can cause problems. The FDA now requires stricter testing for NTI generics - they must be 90% to 111% as strong as the brand, not 80% to 125%. Some people do fine switching, but others don’t. If you’ve had stable levels on one version, it’s safest to stick with it unless your doctor says otherwise.
Can I stop taking my NTI drug if I feel fine?
Never stop or change your dose without talking to your doctor. Even if you feel fine, your blood levels might be too low or too high. For example, people on levothyroxine often feel fine until their TSH spikes - then they suddenly feel exhausted or gain weight. NTI drugs work silently. You can’t feel whether they’re working right - only blood tests can tell you.
Why do I need blood tests so often?
Your body changes. Weight, diet, other meds, stress, even sleep can affect how your body processes NTI drugs. A dose that worked last month might be too high or too low now. Blood tests are your only way to know if the drug is in the safe zone. Skipping them is like driving blindfolded.
Can I take supplements or herbal remedies with my NTI drug?
Many supplements can interfere. St. John’s wort, garlic, ginkgo, and even high-dose vitamin E can affect warfarin. Calcium and iron supplements can block levothyroxine. Always tell your doctor and pharmacist everything you take - even if you think it’s harmless. They’ll check for dangerous interactions.
What should I do if I miss a dose?
Don’t double up. Call your doctor or pharmacist. For warfarin, missing one dose might not be urgent, but for lithium or digoxin, it could be risky. Your provider will tell you whether to skip it or take it late. Never guess - these drugs don’t forgive mistakes.
Is there a list of all NTI drugs?
The FDA doesn’t publish an official list, but experts agree on the most common ones: warfarin, lithium, levothyroxine, digoxin, tacrolimus, phenytoin, carbamazepine, and methotrexate. If your doctor says your drug has a narrow therapeutic index, treat it like a high-risk medication - even if it’s not on a public list.
Next Steps: Take Control
Start today. Write down your drug name and why you take it. Note your next blood test date. Ask your pharmacist if your current pill is the same as last month. Download a simple app to track doses and symptoms. Bring your notes to your next appointment.
You don’t need to be a medical expert. You just need to be consistent. That’s what keeps you safe. That’s what turns a dangerous drug into a life-saving one.









Solomon Ahonsi
3 Feb 2026 at 01:02This whole post is just a scare tactic dressed up as medical advice. I’ve been on warfarin for 5 years and never had an issue switching generics. Pharmacies do it to save money, not to kill people. Stop hyping up the risk like we’re all one missed pill away from bleeding out.