When you take a medication, you expect it to work the same way every time. But with narrow therapeutic index (NTI) drugs, even tiny changes in dosage or formulation can mean the difference between healing and hospitalization. These aren’t your average pills. They’re the kind that keep transplant patients alive, stop seizures, or prevent deadly blood clots. And when it comes to switching from brand to generic, the stakes are higher than most people realize.
What Makes a Drug Have a Narrow Therapeutic Index?
NTI drugs have a razor-thin line between the dose that helps and the dose that harms. A small drop in blood levels might mean the drug stops working. A small rise could cause toxicity-sometimes with life-threatening results. The FDA defines them as drugs where minor changes in concentration can lead to serious side effects, treatment failure, or permanent disability.
Think of it like driving a car with no gas gauge. You know you need fuel, but you can’t tell how much is left. If you’re off by just a few miles per gallon, you could stall-or run out completely. That’s what happens with drugs like warfarin, digoxin, or tacrolimus. Their therapeutic window is so narrow that even a 10% change in blood concentration can trigger problems.
The FDA has officially classified 33 drug products (14 active ingredients) as NTI as of early 2024. These include:
- Immunosuppressants: tacrolimus, cyclosporine, sirolimus
- Anticoagulants: warfarin
- Anti-seizure meds: phenytoin, carbamazepine
- Heart rhythm drugs: digoxin, flecainide
- Thyroid hormone: levothyroxine
- Targeted cancer drugs: axitinib, nilotinib, neratinib
These aren’t obscure drugs. Millions of people rely on them daily. And if you’re one of them, understanding how generics work with NTI drugs isn’t just helpful-it’s essential.
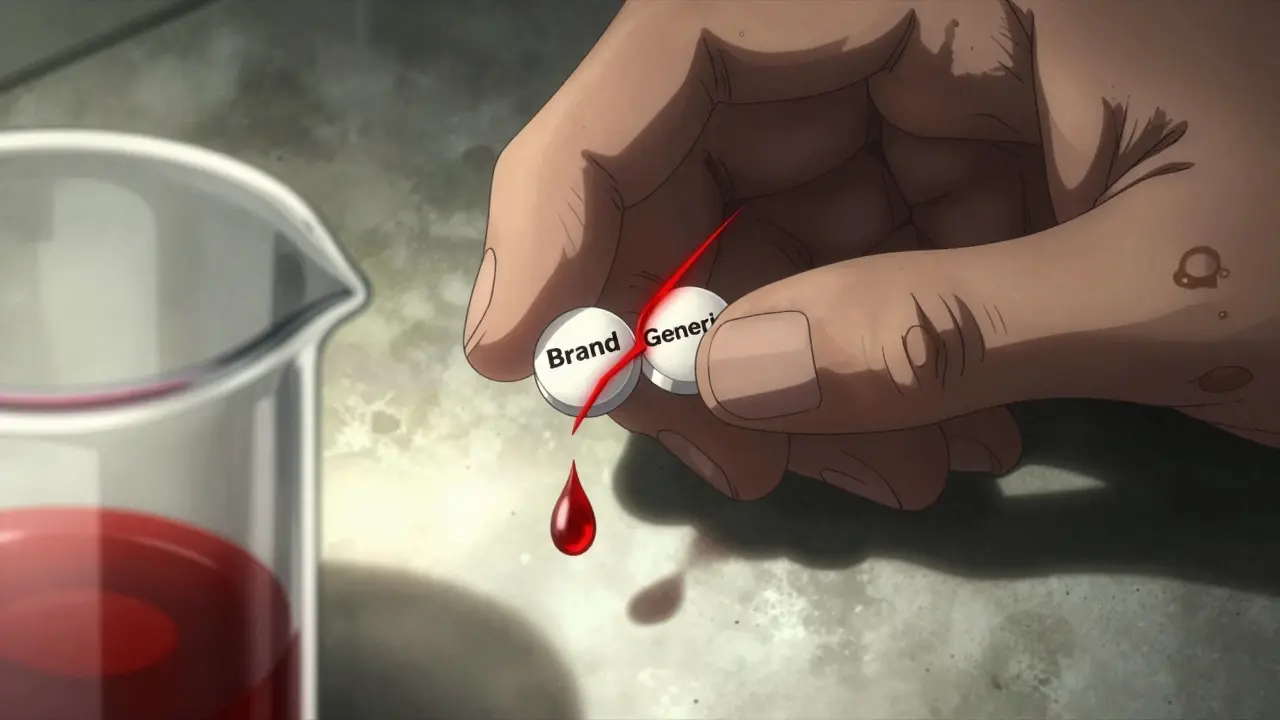
Why Generic NTI Drugs Are Different
Most generic drugs don’t need to be exact copies of the brand. The FDA allows them to be within 80-125% of the brand’s blood concentration and still be considered bioequivalent. That’s a wide range. For many drugs, it’s perfectly safe.
But for NTI drugs, that range is too wide. A 25% variation in blood levels could push someone into toxicity-or make the drug useless. So the FDA tightened the rules. For NTI drugs, the acceptable range is 90-111%. In some cases, if the drug shows very low variability in patients, it tightens even further to 95-105%.
This isn’t just paperwork. It means generic NTI drugs must be tested differently. Instead of a single-dose study in healthy volunteers, manufacturers must run replicate studies-giving the same dose multiple times to the same people-to measure how consistently the drug behaves. This is more expensive and more complex. That’s why fewer companies make generic NTI drugs, and why some brands still dominate the market.
Real-World Risks: When Substitution Goes Wrong
Doctors and pharmacists know the risks. A 2019 national survey found only 28% of pharmacists felt comfortable substituting generic NTI drugs for new prescriptions, compared to 78% for regular drugs. Why? Because they’ve seen what happens.
One kidney transplant patient switched from brand-name Prograf to generic tacrolimus. Three weeks later, his creatinine levels doubled-signaling kidney damage. He ended up hospitalized. Another person on levothyroxine reported wild swings in TSH levels after switching generics, requiring three dose adjustments over six months.
But it’s not all bad. Some patients do fine. A woman with epilepsy has been on generic phenytoin for five years. Her seizures are under control. She saves $300 a month. Her story matters too.
The real issue isn’t whether generics work. It’s whether they work consistently. Switching between different generic versions-or from brand to generic-can cause unpredictable changes in blood levels. That’s why many experts recommend staying on the same manufacturer’s product once you’re stable.
What You Can Do as a Patient
If you take an NTI drug, here’s what you need to know:
- Know your drug. Check if yours is on the FDA’s NTI list. Ask your pharmacist or look up your medication in the FDA’s Drug Shortages database.
- Ask for "dispense as written" on your prescription. This tells the pharmacy not to substitute. You don’t need a reason-just say you prefer consistency.
- Track your levels. If your drug requires therapeutic drug monitoring (TDM), make sure you get tested regularly. Don’t skip blood draws just because you feel fine.
- Report changes. If you notice new symptoms after a switch-fatigue, dizziness, irregular heartbeat, mood changes-contact your doctor immediately. These could be signs of toxicity or underdosing.
- Don’t switch generics unless necessary. Even if two generics are both FDA-approved, they might not behave the same way in your body. Stick with one manufacturer if possible.
Some states have laws that block automatic substitution for NTI drugs. As of 2023, 42 states restrict it in some way. But the rules vary. In some places, pharmacists can still switch unless the doctor writes "DAW" (dispense as written). In others, substitution is banned entirely. Know your state’s rules.
Why This Matters for Your Health
NTI drugs are used in the most vulnerable populations: transplant recipients, elderly patients with heart conditions, people with epilepsy or thyroid disorders. These groups often take multiple medications, increasing the risk of dangerous interactions. A single change in one drug can throw off the whole system.
Patients with diabetes or heart failure are at higher risk of drug-related problems with NTI drugs-up to 31% more likely, according to NIH data. That’s not a small number. It’s a red flag.
And it’s not just about cost. Yes, generics save money. But if switching causes a hospital visit, the cost of care skyrockets. A single readmission for drug toxicity can cost over $15,000. That’s far more than the savings from a cheaper pill.
Health systems are starting to catch on. The Joint Commission now requires documentation of therapeutic drug monitoring for NTI drugs as part of medication safety standards. Hospitals are training pharmacists in specialized NTI protocols. The American Society of Health-System Pharmacists recommends at least 16 hours of annual training for pharmacists managing these drugs.
The Future of NTI Drugs
The market for NTI drugs is growing fast. It was worth $137.4 billion in 2022 and is projected to hit $185.7 billion by 2027. Why? Because newer cancer drugs, biologics, and targeted therapies often have narrow therapeutic indices. More patients will need these drugs-and more will need to understand them.
One big shift coming: pharmacogenomics. By 2028, 40% of NTI drug prescriptions may include genetic testing to predict how a person metabolizes the drug. That means dosing could be personalized-not just based on weight or age, but on your DNA.
The FDA is also working to standardize NTI definitions globally. Right now, the U.S., Europe, and Japan all have different criteria. That creates headaches for drug makers and confusion for patients who travel or get medications from abroad.
For now, the best advice is simple: know your drug, know your dose, know your blood levels. Don’t let cost be the only factor when your life depends on consistency.
Common Questions About NTI Drugs and Generics
Are all generic drugs unsafe for NTI medications?
No. Many generic NTI drugs are safe and effective when manufactured to the FDA’s tighter bioequivalence standards. The issue isn’t generics themselves-it’s switching between different versions. Once you’re stable on a specific generic, staying on it is usually fine. Problems arise when you switch brands, or when a pharmacy substitutes without your doctor’s knowledge.
Can I ask my doctor to write "dispense as written" on my prescription?
Yes, absolutely. You don’t need a medical reason. Just say you want to avoid any changes in your medication. Many patients do this with NTI drugs, and doctors support it. The FDA encourages prescribers to use "dispense as written" when consistent product sourcing is needed for safety.
Why do some people do fine on generic NTI drugs while others don’t?
Everyone’s body absorbs and processes drugs differently. Factors like age, liver function, other medications, and even diet can affect how a drug behaves. Some people have very stable metabolism and don’t notice small differences. Others are more sensitive. That’s why therapeutic drug monitoring is so important-it tells you what’s really happening in your bloodstream, not what you feel.
What should I do if my insurance switches my NTI drug to a different generic?
Contact your doctor right away. Ask them to request a prior authorization for your original brand or generic. If that’s not possible, ask for a blood test to check your drug levels. Don’t wait for symptoms to appear. Even if you feel fine, your levels might be drifting into a dangerous range.
Is there a list of all NTI drugs I can check?
Yes. The FDA publishes product-specific guidances for generic NTI drugs. These list the approved active ingredients and their bioequivalence requirements. You can find them on the FDA’s website under "Drug Approvals and Databases" → "ANDA Submissions" → "Product-Specific Guidance for Generic Drug Development." Your pharmacist can also help you identify if your drug is classified as NTI.
Next Steps for Patients and Caregivers
If you or someone you care for takes an NTI drug, start with three simple actions:
- Check the drug’s classification. Is it on the FDA’s NTI list?
- Review your prescription. Does it say "dispense as written"? If not, ask your doctor to add it.
- Set a reminder for your next blood test. Don’t wait for symptoms. Regular monitoring is your safety net.
NTI drugs aren’t dangerous because they’re weak. They’re dangerous because they’re powerful. And when used correctly-with awareness, consistency, and monitoring-they save lives. The goal isn’t to avoid generics. It’s to make sure every pill you take does exactly what it’s supposed to-without surprises.






Luke Davidson
22 Jan 2026 at 15:17Man I never realized how wild it is that some pills can make or break you with a tiny switch
My cousin’s on tacrolimus after his transplant and they switched generics once-ended up in the ER with kidney numbers through the roof
Now he only takes the brand and his doc signed off on it
Why risk it when your life’s on the line?