It’s easy to think that if a drug makes you feel sick, you’re allergic to it. But here’s the truth: most people who say they have a drug allergy don’t actually have one. In fact, 9 out of 10 people who think they’re allergic to penicillin can take it just fine. The problem? They’re confusing a side effect with a real allergy. And that mistake can cost you - in money, time, and even your health.
What’s the Difference?
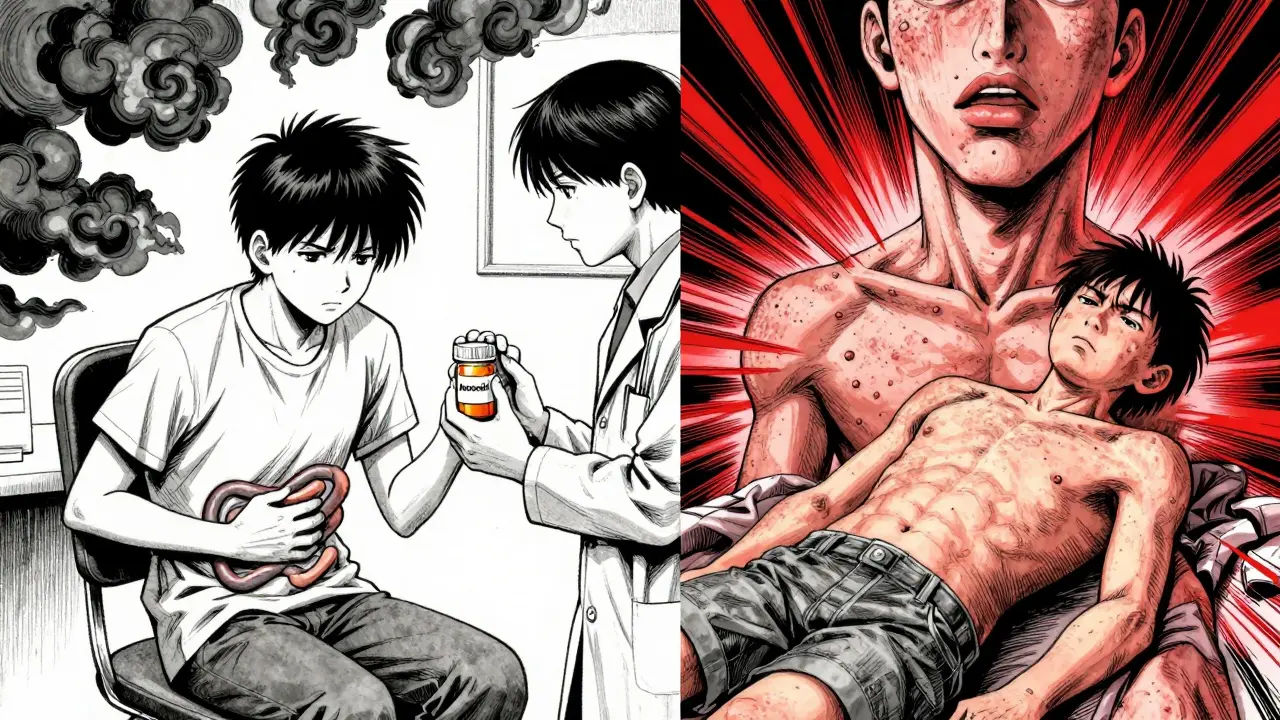
A side effect is a known, predictable reaction to a drug because of how it works in your body. For example, antibiotics like amoxicillin can upset your stomach. That’s not because your immune system is attacking the drug - it’s because the drug is killing off good bacteria in your gut. Nausea, dizziness, headaches, and dry mouth are classic side effects. They’re listed in the patient info pamphlet for a reason: they happen to a lot of people, and they usually go away if you stop the drug or lower the dose.
A true drug allergy is an immune system overreaction - your body mistakes the drug for a dangerous invader and launches a full attack. This isn’t just feeling queasy. This is your body releasing histamine, swelling up, breaking out in hives, or going into shock. It’s not about how much you took - it’s about your immune system’s response. And once it happens, it can get worse every time you take the drug again.
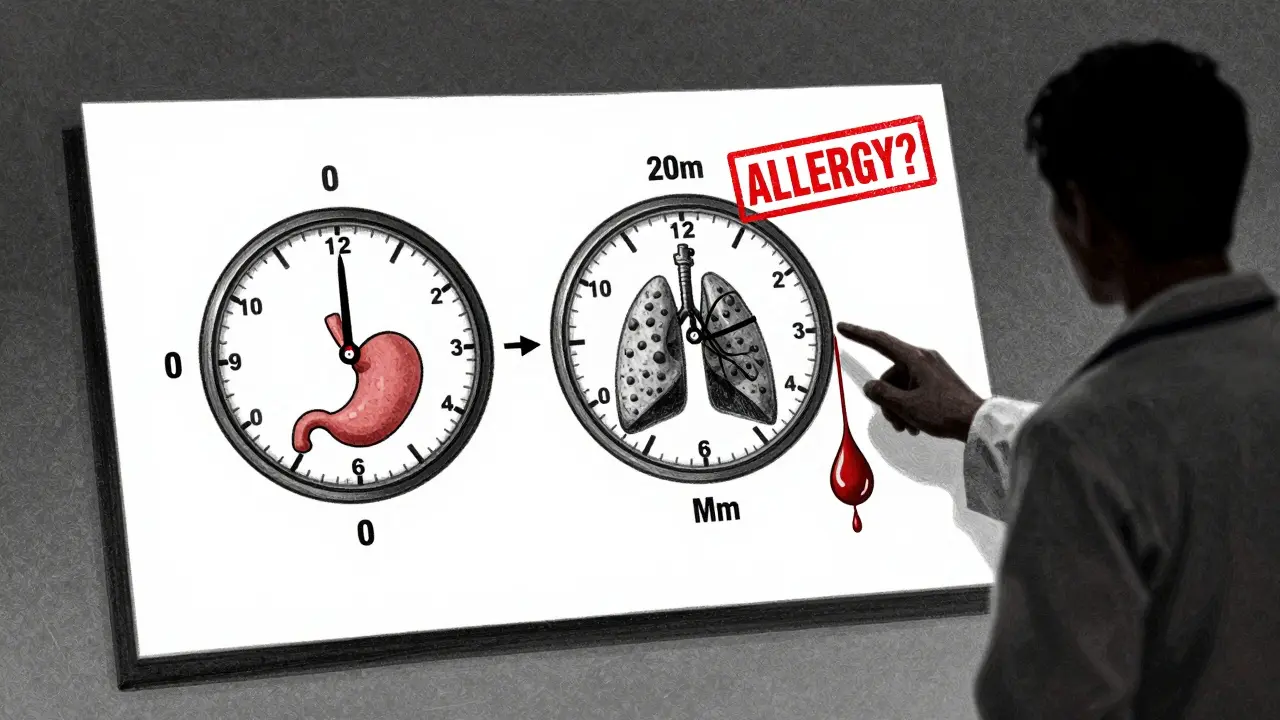
Timing Matters
When symptoms show up tells you a lot. Side effects usually appear soon after you start the drug - sometimes within hours. They might get worse if you take more, or better if you take less. You might feel a bit dizzy after your first dose of blood pressure meds. That’s common. It doesn’t mean you’re allergic.
True allergies have clear timing patterns:
- Immediate reactions - within 1 hour. Think hives, swelling of the lips or tongue, trouble breathing, or a sudden drop in blood pressure. These are IgE-mediated. Penicillin, sulfa drugs, and some painkillers like ibuprofen can trigger these.
- Delayed reactions - days to weeks later. A rash that spreads slowly over your chest and back? That’s often T-cell driven. It can look like measles or a sunburn. In rare cases, it can turn into something deadly like DRESS (Drug Reaction with Eosinophilia and Systemic Symptoms) or Stevens-Johnson Syndrome. These show up 7-14 days after starting the drug - sometimes even later.
If you broke out in hives 20 minutes after taking amoxicillin? That’s a red flag. If you got a stomachache two hours after taking aspirin? Probably not.
Symptom Patterns Are Key
Side effects usually stick to one system. Stomach upset? That’s GI. Headache? That’s neurological. Dizziness? That’s vestibular. Simple.
True allergies? They rarely stay in one place. The immune system doesn’t just hit one organ - it hits multiple. Here’s what a real allergic reaction often looks like:
- Hives + swelling of the throat
- Rash + wheezing + vomiting
- Itchy skin + low blood pressure + rapid heartbeat
According to data from the Mayo Clinic, 87% of confirmed drug allergies involve at least two body systems. Side effects? Only 22% do. If you’re only nauseous, you’re likely not allergic. If you’re nauseous and your face is swelling? That’s an emergency.
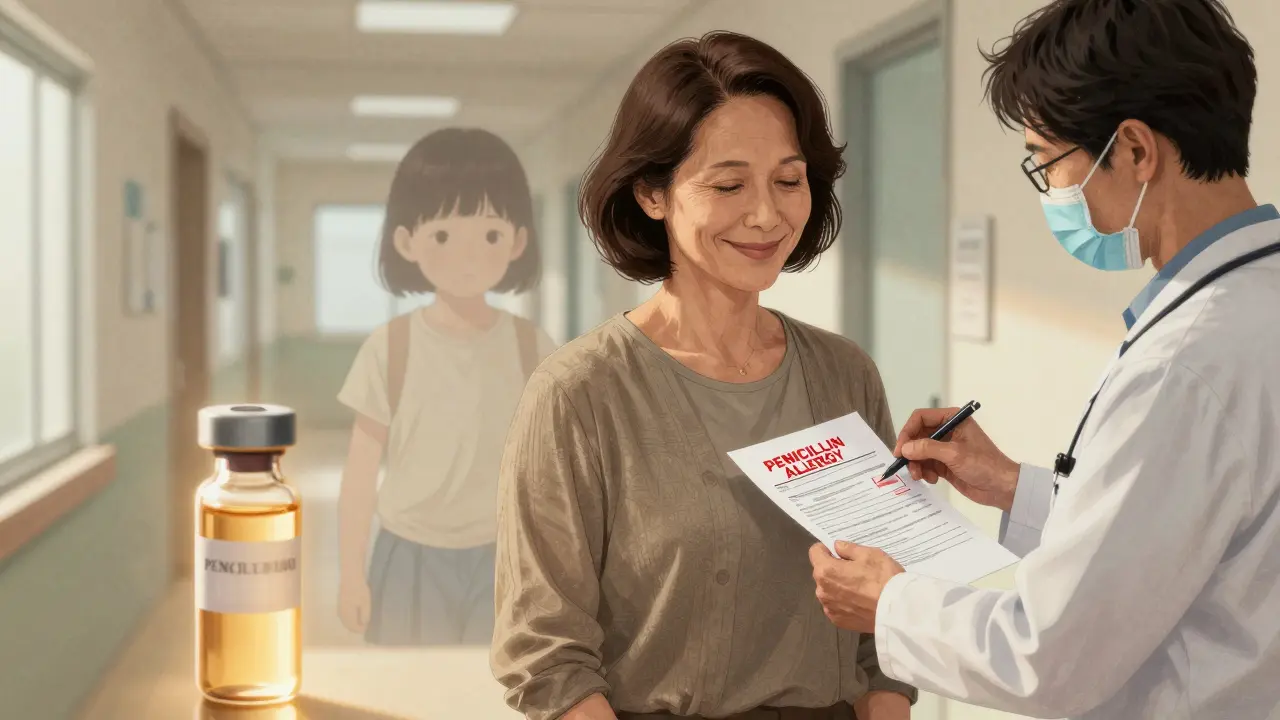
What About Penicillin?
Penicillin is the classic example. About 10% of Americans say they’re allergic to it. But when they’re tested - with skin tests or oral challenges - 90-95% turn out not to be allergic at all. Why? Because they had nausea or diarrhea after taking it as a kid and assumed it was an allergy. Or their parent told them they were allergic, and they never questioned it.
Here’s the scary part: people with a mislabeled penicillin allergy are more likely to get stronger, broader-spectrum antibiotics. Those drugs are more expensive, harder on your gut, and more likely to cause real problems like C. difficile infections. A 2022 JAMA study found these patients had 69% higher rates of C. diff and stayed in the hospital 30% longer.
And here’s the good news: if you think you’re allergic to penicillin, you can get tested. Skin tests are 95% accurate. A supervised oral challenge - where you take a small dose under medical supervision - is the gold standard. Most people pass. And if they do? Their medical records get updated. Future doctors stop avoiding penicillin. And you get better, cheaper, safer treatment.
What About Other Drugs?
It’s not just penicillin. Sulfa drugs, NSAIDs like ibuprofen, and even some chemotherapy agents can cause true allergies. But here’s the catch: not every bad reaction is an allergy.
- Aspirin: Nausea? Side effect. Rash? Possibly allergy. Trouble breathing after taking it? That could be a true allergy - especially if you also have asthma. This is called aspirin-exacerbated respiratory disease.
- Statins: Muscle aches? Common side effect. Liver enzymes up? Also common. But if you get swelling, hives, or trouble breathing? That’s rare - but real.
- Chemotherapy: Fatigue, hair loss, vomiting? Expected side effects. But if you get low blood pressure, chest pain, or a rash within minutes of infusion? That’s an infusion reaction - and it’s often immune-mediated.
The key? Look at the pattern. Was it just one symptom? Likely a side effect. Multiple systems? Time to get checked.
What Should You Do?
If you’ve ever had a bad reaction to a drug, don’t just assume it’s an allergy. Ask yourself:
- What happened? (Hives? Swelling? Trouble breathing? Or just nausea?)
- When did it happen? (Within an hour? Or days later?)
- Did it happen again? (Did the same reaction happen the next time you took it?)
- Did other symptoms show up? (Skin + breathing + GI? That’s a red flag.)
If you’re unsure, talk to your doctor. Ask for a referral to an allergist. They can do skin tests, blood tests (like the new Penicillin ImmunoCAP test), or even a controlled challenge. These aren’t risky if done right - and they can save you from unnecessary restrictions.
And if you’re a patient with a long-standing "allergy" label? Don’t be afraid to get it re-evaluated. A 2023 study in the Journal of Allergy and Clinical Immunology showed that 78% of patients who got retested could safely use the drug they’d avoided for years. One woman in Melbourne told her doctor she was allergic to penicillin because she got a rash as a child. She was 47. After testing, she got a clean bill of health. Two months later, she got a simple infection - and took penicillin. It worked. No side effects. No problems.
Why This Matters
Wrong labels aren’t just inconvenient - they’re dangerous. When doctors avoid penicillin because of a mislabeled allergy, they turn to broader-spectrum antibiotics. Those drugs kill more good bacteria. They cost more. They increase antibiotic resistance. And they make you more likely to get dangerous infections.
The CDC estimates that mislabeling penicillin allergies costs the U.S. healthcare system over $1 billion a year. Hospitals that have implemented formal allergy review programs - led by pharmacists and allergists - have cut inappropriate antibiotic use by 27%. That’s not just money saved. It’s lives saved.
The FDA now requires drug labels to clearly separate "side effects" from "allergies." And by 2025, all electronic health records must distinguish between them too. This isn’t bureaucracy - it’s patient safety.
Bottom Line
Not every bad reaction is an allergy. Most aren’t. But if you have hives, swelling, trouble breathing, or a rash that spreads fast - especially with other symptoms - don’t ignore it. Get it checked. And if you’ve been avoiding a drug for years because you "think" you’re allergic? Ask your doctor if you can get tested. You might be surprised. And you might just get better care - without the risk.










Ariel Edmisten
8 Feb 2026 at 02:51Most people don’t realize how often side effects get mislabeled as allergies. I had a stomachache after penicillin as a kid. Turned out I just had a sensitive gut. Got tested at 30 - turned out fine. Saved me from years of unnecessary antibiotics.
Simple as that.