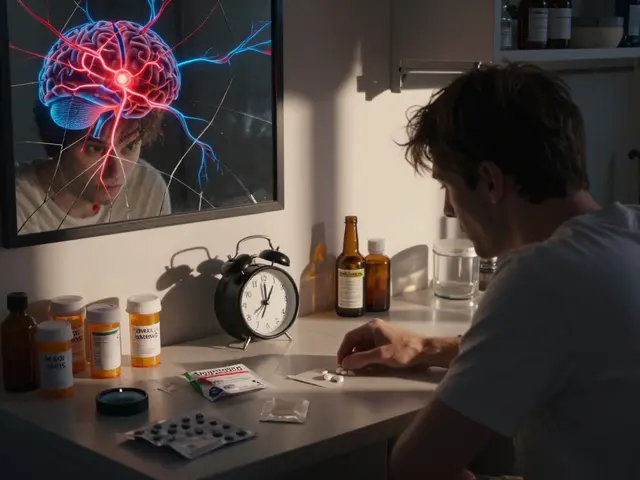
Imagine this: You’re a pharmacist. A patient walks in with a new prescription for a blood thinner. You check their history and see they’re already on another anticoagulant. The doctor didn’t know. If you’re working without access to their full medical record, you might just fill the script-and risk a dangerous interaction. But if your pharmacy system talks directly to the doctor’s EHR? You catch it before it happens. That’s not science fiction. It’s happening right now, in pockets across the U.S. and Australia. And it’s changing how prescriptions are handled-for the better.
What EHR Integration Actually Does for Pharmacies and Providers
EHR integration means the pharmacy’s system and the provider’s electronic health record talk to each other in real time. It’s not just about sending a prescription electronically. That’s been around for years. True integration lets pharmacists see the patient’s full history: lab results, allergies, other meds, recent hospital visits. And it lets doctors see what the pharmacist did-like adjusting a dose, flagging a duplicate, or counseling the patient.
This isn’t just convenient. It saves lives. A 2022 study showed that when pharmacists had access to EHR data, they caught and fixed 4.2 medication-related problems per patient visit. Without access? That number dropped to 1.7. That’s more than double the number of errors prevented.
It also cuts down on delays. Before integration, a prior authorization request could take days. Now, with systems like Surescripts connecting pharmacies to insurers and providers, some approvals happen in under four hours. One pharmacist on Reddit said their team went from 48 hours of back-and-forth calls to just four hours of automated processing.
How the Technology Works: Standards That Make It Possible
This isn’t magic. It’s built on specific, agreed-upon technical rules. The two biggest players are NCPDP SCRIPT and HL7 FHIR.
NCPDP SCRIPT (version 2017071) is the old workhorse. It’s what sends the prescription from the doctor’s computer to the pharmacy. It’s reliable, widely used, and handles the basics: drug name, dose, quantity, instructions.
But SCRIPT alone doesn’t give you context. That’s where HL7 FHIR comes in. FHIR (Fast Healthcare Interoperability Resources) is the new standard. It lets systems exchange richer data: lab values, diagnoses, care plans, even patient-reported symptoms. The Pharmacist eCare Plan (PeCP) is a FHIR-based format designed just for pharmacists to share their clinical insights back to the provider.
These systems connect through secure APIs. They use OAuth 2.0 to verify who’s logging in, HTTPS to protect data in transit, and AES-256 encryption to keep records safe when stored. All of this meets HIPAA and the 21st Century Cures Act rules-no data sharing is allowed without strict security.
And the scale is massive. Surescripts alone processes over 22 billion transactions a year. That’s prescriptions, eligibility checks, prior authorizations-all flowing between systems. But here’s the catch: only 15-20% of pharmacies have true bidirectional integration. Most still only send prescriptions out. They don’t get the full picture back.
Why So Few Pharmacies Are Integrated-And What’s Holding Them Back
It’s not that pharmacies don’t want to integrate. It’s that the cost and complexity are brutal.
For an independent pharmacy, setting up integration can cost between $15,000 and $50,000 upfront. Then there’s $5,000 to $15,000 a year just to keep it running. That’s more than most small pharmacies make in profit in a quarter.
Then there’s time. Pharmacists average just 2.1 minutes per patient interaction. Even if they have access to EHR data, they don’t have time to dig through it. One survey found 68% of pharmacists say they simply don’t have enough time to review the information.
And even when they do, the data doesn’t always make sense. There are over 120 different EHR systems and 50 pharmacy management platforms in the U.S. None of them talk the same language. One system might label a drug as “metoprolol succinate,” another as “toprol-xl.” Mapping those differences takes hours of manual work-and many systems still can’t do it automatically.
Only 3 out of 127 community pharmacies surveyed in Wisconsin had formal agreements with health systems to access EHRs. That’s less than 2.5%. Meanwhile, 89% of hospital-based pharmacies are integrated. The gap isn’t just technical-it’s structural. Big health systems have the budget and leverage. Independent pharmacies don’t.

Who’s Winning: Real-World Success Stories
Despite the barriers, some places are making it work.
In East Tennessee, a proof-of-concept study connected 12 independent pharmacies with Epic EHR systems using PeCP and FHIR. Over three months, pharmacists made 1,847 clinical interventions-like adjusting doses, spotting drug interactions, or reminding patients to refill. Providers accepted 92% of those suggestions. That’s not just efficiency. That’s better care.
In Australia, the My Health Record system cut preventable hospitalizations by 27% by giving pharmacists and doctors access to the same data. For patients on four or more chronic medications, adverse drug events dropped by 34%.
And the numbers add up. One study found that integrated systems saved $1,250 per patient per year by reducing unnecessary prescriptions, hospital readmissions, and ER visits. Another showed medication adherence improved by 23%. That’s not a small win. That’s a system-wide shift.
Pharmacists who use integrated systems say they feel like real members of the care team-not just pill counters. One said, “I used to just fill scripts. Now I’m the one catching the mistakes no one else sees.”
Commercial Tools Making Integration Possible
You don’t have to build this from scratch. Several platforms offer ready-made solutions:
- Surescripts: The biggest player. Handles 97% of U.S. pharmacies. Offers Medication History, Eligibility Checks, and Prior Authorization-all through one API. Costs around $0.03-$0.05 per transaction.
- SmartClinix: A pharmacy-specific EMR with built-in EHR integration. Starts at $199/month. Users love its Epic connection but say the learning curve is steep.
- DocStation: Focuses on provider networks and billing. Starts at $249/month. Great for clinics that want to manage multiple pharmacies.
- UpToDate: Not a pharmacy system, but integrates with 40+ EHRs to deliver drug info directly into clinician workflows. Useful for providers, not pharmacists directly.
None of these are cheap. But compared to the cost of building your own interface? They’re a bargain. And they come with support-something most small pharmacies can’t afford to do alone.

The Future: What’s Coming Next
The push for integration is only getting stronger.
Medicare Part D now requires plans to integrate medication therapy management (MTM) by 2025. California’s SB 1115 mandates EHR integration for MTM by 2026. The Office of the National Coordinator for Health IT wants 50% of community pharmacies integrated by 2027.
The next big leap? AI. CVS and Walgreens are testing machine learning tools that scan integrated EHR-pharmacy data to predict which patients are at risk for non-adherence or dangerous interactions. Early results show a 37% improvement in identifying problems before they happen.
But the biggest hurdle isn’t tech. It’s payment. Right now, only 19 states reimburse pharmacists for EHR-based care coordination. That’s a dealbreaker for small pharmacies. As one expert put it: “Without sustainable payment models, EHR integration will remain a luxury, not a standard.”
The 2023 Pharmacy and Medically Underserved Areas Enhancement Act proposes Medicare reimbursement for pharmacist services delivered through integrated systems. If it passes, it could be the turning point.
What This Means for Patients
At the end of the day, this isn’t about technology. It’s about you.
If you’re on multiple medications, have a chronic condition, or take drugs with narrow safety margins, integrated EHR-pharmacy systems mean fewer mistakes, fewer hospital trips, and more personalized care. Your pharmacist won’t just hand you a bottle-they’ll know your full story.
And if you’re a provider? You’ll get alerts before a patient ends up in the ER. You’ll know if your prescription was filled, if the patient took it, and if there’s a better option.
This is the future of care: connected, proactive, and patient-centered. It’s not here everywhere yet. But it’s coming. And when it does, no one will wonder why it took so long.
What is EHR integration in pharmacy?
EHR integration in pharmacy means connecting a pharmacy’s system directly to a patient’s electronic health record used by doctors and hospitals. This allows pharmacists to see the patient’s full medical history-including allergies, lab results, and other medications-and share clinical insights back to the provider. It’s not just electronic prescribing; it’s two-way communication that improves safety and coordination.
Why don’t all pharmacies have EHR integration?
Cost is the biggest barrier. Independent pharmacies face $15,000-$50,000 in setup fees and $5,000-$15,000 annually to maintain integration. Time is another issue-pharmacists have only 2.1 minutes per patient on average, leaving little room to review complex EHR data. Technical challenges also exist, as over 120 EHR systems and 50 pharmacy platforms don’t always speak the same language. Only 15-20% of U.S. pharmacies have true bidirectional integration.
How does EHR integration reduce medication errors?
Integrated systems flag drug interactions, duplicate prescriptions, and incorrect dosages in real time. Pharmacists with EHR access identify 4.2 medication-related problems per patient visit-more than double the rate without access. Automated alerts and clinical decision support reduce errors by up to 48%, according to UpToDate. Studies show a 31% drop in medication-related hospital readmissions when integration is in place.
What standards are used for pharmacy-EHR communication?
The NCPDP SCRIPT standard (version 2017071) handles prescription transmission. HL7 FHIR Release 4 (R4) enables richer data exchange, like lab results and care plans. The Pharmacist eCare Plan (PeCP), built on FHIR, lets pharmacists share clinical notes back to providers. These systems use OAuth 2.0 for secure login, HTTPS for data transfer, and AES-256 encryption for stored data-all required by HIPAA and the 21st Century Cures Act.
Is EHR integration worth the cost for small pharmacies?
It depends. For small pharmacies, the upfront cost ($15K-$50K) and annual fees ($5K-$15K) are steep. But the return comes in reduced errors, fewer readmissions, and improved patient outcomes. Some states now reimburse pharmacists for EHR-based care coordination. Without reimbursement, it’s a financial risk. With it, integration can become a competitive advantage and a revenue stream.
What’s the biggest barrier to widespread adoption?
The biggest barrier is payment. Only 19 states reimburse pharmacists for EHR-based services like medication therapy management. Without reimbursement, pharmacies can’t justify the cost. Even with proven benefits-like 23% higher adherence and $1,250 annual savings per patient-many independent pharmacies can’t afford to invest unless they get paid for the value they provide.










ian septian
7 Dec 2025 at 21:44This is huge. Pharmacies catching errors before they happen? Yes please.
More of this, less guesswork.