When you pick up a generic inhaler, patch, or injection, you assume it works just like the brand-name version. But getting there isn’t as simple as copying a pill. For complex delivery systems like these, bioequivalence isn’t just about matching blood levels-it’s about proving the drug reaches the right place in the body, at the right time, in the right amount. And that’s where things get complicated.
Why Bioequivalence Isn’t the Same for Inhalers, Patches, and Injections
For oral pills, bioequivalence is straightforward: measure how much drug shows up in your bloodstream (AUC) and how fast it gets there (Cmax). If the generic’s numbers fall between 80% and 125% of the brand, it’s approved. But that rule doesn’t work for inhalers, patches, or injectables because the drug doesn’t always enter the bloodstream the same way-or even at all. Take inhalers. The goal isn’t to flood your blood with medication. For asthma or COPD treatments like albuterol or fluticasone, the drug needs to land in your lungs. If the particle size is off by even a micron, or the spray pattern changes slightly, the medicine might hit your throat instead of your airways. That’s not bioequivalence-it’s a wasted dose. The FDA now requires inhaler generics to match the brand in particle size (90% of particles between 1-5 micrometers), dose uniformity (within 75-125% of labeled amount), and even the temperature and shape of the spray plume. One generic albuterol inhaler got rejected because its plume was 2°C warmer than the original. That tiny difference changed how the drug dispersed in the airway. Transdermal patches are another story. These are designed to release drug slowly through your skin over hours or days. You can’t just measure Cmax and call it done. A patch that releases 10% more drug in the first two hours might cause side effects, even if the total exposure (AUC) matches. The FDA requires in vitro tests showing identical release rates at every time point, plus matching skin adhesion and residual drug content. For nicotine patches, this works well. For pain patches like fentanyl, even small differences can be dangerous. Injectables are the toughest. If it’s a simple saline solution, standard blood tests work fine. But for liposomal doxorubicin, nanoparticle albumin-bound paclitaxel, or long-acting insulin glargine, the drug’s physical structure matters as much as the chemical. The particle size must be within 10%, the polydispersity index below 0.2, and the zeta potential within 5mV. Change any of those, and your body treats the drug like a foreign invader-slowing absorption, triggering immune reactions, or reducing effectiveness. The FDA rejected a generic version of Bydureon BCise because the auto-injector mechanism delivered the drug differently, even though the chemical formula was identical.The Cost and Time to Prove Bioequivalence
Developing a generic pill costs $5-10 million and takes 18-24 months. For complex delivery systems? It’s $25-40 million and 36-48 months. Why? Because you need specialized equipment: cascade impactors for inhalers ($150,000-$300,000), Franz diffusion cells for patches ($50,000-$100,000), and nanoparticle analyzers for injectables ($200,000+). You also need teams trained in physicochemical characterization, pharmacokinetic modeling, and regulatory science. Most small companies can’t afford it. And even then, approval rates are low. Only 38% of inhaler generics get approved, compared to 78% for oral drugs. Transdermal patches have a 52% approval rate. Complex injectables? 58%. That’s not because the science is flawed-it’s because the bar is set high. The FDA rejected a generic Advair Diskus in 2019 because the fine particle fraction was just 3% lower than the brand. That might sound minor, but in lungs, 3% can mean more hospital visits.How Regulators Are Adapting
Regulatory agencies aren’t stuck in the past. The FDA, EMA, and WHO now have detailed, product-specific guidance for each delivery system. The FDA’s 2022 inhaler guidance, EMA’s 2019 inhaled product guidelines, and their 2018 complex injectables document all move away from relying solely on blood tests. Instead, they use a totality-of-the-evidence approach. That means combining:- In vitro testing (particle size, release rate, plume geometry)
- Physicochemical characterization (particle shape, surface charge, stability)
- Pharmacokinetic studies (when systemic absorption matters)
- Pharmacodynamic endpoints (like FEV1 for inhalers or pain relief for patches)
- Real-world device performance (how the injector clicks, how the patch sticks)
Real-World Failures and Successes
Not every generic makes it. In 2021, a company spent $45 million developing a generic version of Bydureon BCise, only to have the FDA reject it over injector mechanics. Another generic insulin glargine took 42 months and 17 formulation tries just to get the particle size right. But success stories exist. Teva’s generic ProAir RespiClick got approved in 2019 after using scintigraphy imaging to prove identical lung deposition. Within 18 months, it captured 12% of the market. Why? Because it didn’t just match the drug-it matched the experience.What’s Next for Bioequivalence?
The future is in modeling. In 2022, 65% of complex generic submissions included physiologically-based pharmacokinetic (PBPK) models-up from 22% in 2018. These computer simulations predict how a drug behaves in the body based on its physical properties, reducing the need for expensive human trials. The FDA is also testing new approaches for monoclonal antibody injections, which are biologics, not small molecules. These require different rules entirely. And there’s growing concern about “biocreep”-where multiple generations of generics, each slightly different, might accumulate enough variation to affect safety over time.
Why This Matters to You
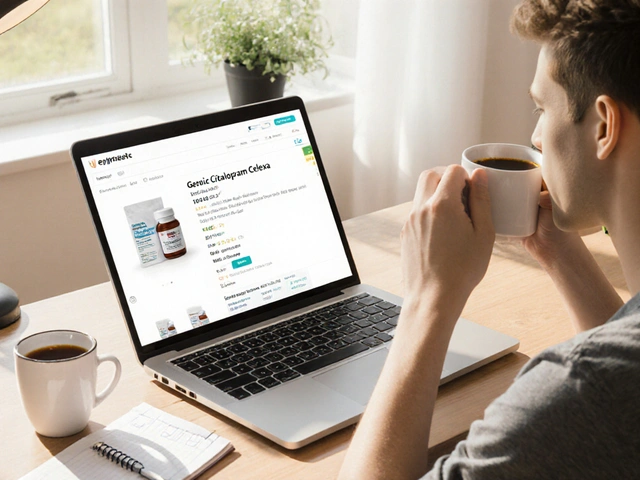
If you use an inhaler, patch, or long-acting injection, bioequivalence rules protect you. They stop cheap knockoffs from failing silently. But they also mean fewer generics enter the market. Only 15% of complex delivery system prescriptions are filled with generics-even though they make up 30% of all prescriptions. That’s because development costs are so high that only a few big companies (Teva, Mylan, Sandoz) can afford to play. The result? You might pay more for a generic inhaler than you would for a brand-name pill. But you’re also getting a product that’s been tested not just for chemistry, but for how it actually works in your body.What You Can Do
If your doctor prescribes a complex delivery system, ask if a generic is available. If not, ask why. Sometimes it’s because no one has passed the bioequivalence test yet. Other times, it’s because the brand still holds a patent or has exclusive rights. Don’t assume generics are always cheaper or better-they’re only better if they’re truly equivalent. Stay informed. The FDA and EMA update their guidance documents quarterly. If you’re a patient, caregiver, or healthcare provider, you can access these for free. They’re not just for scientists-they’re for anyone who wants to understand why a generic might not work the same way, even if it looks identical.What is bioequivalence for inhalers, patches, and injections?
Bioequivalence for these delivery systems means proving that a generic product delivers the active drug to the target site-like the lungs, skin, or bloodstream-at the same rate and extent as the brand-name version. Unlike oral pills, this often requires more than just blood tests. It includes matching particle size, release rate, device performance, and sometimes even clinical outcomes like lung function or pain relief.
Why are generic inhalers harder to approve than pills?
Because inhalers rely on precise particle size, spray pattern, and inhalation technique to deliver medicine to the lungs. If the particles are too big, they hit the throat. If the spray is too hot or too forceful, the drug doesn’t reach deep enough. Even small differences in the device’s mechanics can reduce effectiveness. The FDA requires in vitro tests and sometimes lung imaging to prove equivalence, which is far more complex than measuring blood levels.
Can a generic patch have the same drug but still not work?
Yes. A patch might contain the exact same chemical, but if the adhesive changes, the drug release rate slows down, or the patch doesn’t stick as well, the amount of drug entering your body over time can be different. For drugs like fentanyl or nicotine, even a 10% variation in release rate can cause withdrawal symptoms or overdose risk. That’s why regulators require in vitro release testing at every time point.
Why do complex injectables need particle size testing?
For injectables like liposomal doxorubicin or nanoparticle albumin-bound paclitaxel, the drug is encased in tiny particles that control how and where it’s released in the body. If the particle size changes, the immune system may clear it faster, or the drug might not reach the tumor. The FDA requires particle size within 10% of the brand, a polydispersity index under 0.2, and matching surface charge-all to ensure the drug behaves the same way in your body.
Are generic inhalers and patches cheaper?
Sometimes, but not always. Because development costs are so high ($25-40 million), only a few companies make these generics. That limits competition, so prices don’t drop as much as with oral drugs. Some generic inhalers cost nearly as much as the brand. But when generics do enter the market-like Teva’s ProAir RespiClick-they can capture significant market share and eventually bring prices down.










Fabio Raphael
26 Dec 2025 at 00:18I never realized how much engineering goes into something as simple as an inhaler. I thought generics were just cheaper versions of the same thing, but now I get it-this isn’t just chemistry, it’s physics, fluid dynamics, and user experience all rolled into one. That 2°C difference in spray temperature? Wild. Makes you wonder how many people are getting subpar doses without even knowing it.
Thanks for laying this out so clearly. I’m going to ask my pulmonologist about the specific device I’m using now.