When you pick up a prescription, you might be surprised by the price-even if you have insurance. That’s because your plan doesn’t cover all drugs the same way. Instead, it uses something called a formulary tier system to decide how much you pay. Understanding these tiers isn’t just helpful-it can save you hundreds or even thousands of dollars a year.
What Is a Formulary, and Why Do Tiers Exist?
A formulary is a list of prescription drugs your health plan covers. It’s not random. Insurance companies, working with Pharmacy Benefit Managers (PBMs) like Express Scripts and CVS Caremark, build these lists to control costs while still giving you access to necessary medications. They group drugs into tiers based on price, effectiveness, and whether a cheaper generic version exists. The goal? Encourage you to use drugs that are both effective and affordable. A Tier 1 drug might cost you $5. A Tier 3 drug? $80. Same condition. Same doctor’s order. Totally different price. That’s the power-and the problem-of tiered formularies.Tier 1: The Lowest Cost, Usually Generics
Tier 1 is where you want to be. This tier includes mostly generic medications that have been around for years, with proven safety and low cost. Think blood pressure pills like lisinopril, cholesterol meds like atorvastatin, or diabetes drugs like metformin. In most commercial plans, Tier 1 copays range from $0 to $15 for a 30-day supply. Medicare Part D plans list Tier 1 as the lowest copayment tier, specifically for generic drugs. These are the drugs your plan wants you to use because they’re cheap, effective, and widely available. Here’s the catch: not all generics are equal. Your plan picks which ones are preferred. If your doctor prescribes a generic that’s not on Tier 1, you might pay more-even if it’s the same active ingredient. That’s why checking your formulary before filling a script matters.Tier 2: Preferred Brand-Name Drugs
Tier 2 includes brand-name drugs that your plan has negotiated better deals on. These are often newer than Tier 1 generics but still have competitors on the market. For example, a brand-name version of a common antidepressant like sertraline might be in Tier 2 if a generic exists but the brand is still widely used. Copays here typically run $20 to $40 for a 30-day supply. Medicare calls this tier “medium copayment” for preferred brand-name drugs. The key word is preferred. That means your insurer has a contract with the drugmaker to get a discount-or rebate-in exchange for putting it in this lower tier. But here’s what trips people up: just because a drug is brand-name doesn’t mean it’s in Tier 2. Some brand-name drugs are in Tier 3. Why? Because they’re more expensive, or there’s a cheaper alternative your plan prefers.Tier 3: Non-Preferred Brand-Name Drugs
Tier 3 is where things get expensive. These are brand-name drugs without a generic version, or ones your plan doesn’t recommend because cheaper options exist. Think of drugs for conditions like rheumatoid arthritis or certain types of migraines where only one or two brands are commonly prescribed. Copays for Tier 3 drugs average $50 to $100 per 30-day supply. In some plans, you might even pay coinsurance-say, 30% of the drug’s total cost-instead of a flat fee. That means if the drug costs $300, you pay $90. Many patients are shocked when their doctor prescribes a drug they’ve used for years, only to find out it’s been moved to Tier 3. That happens. Formularies change quarterly. Your plan might have signed a new deal with a competitor’s manufacturer, pushing your drug out of favor.
Tier 4 and 5: Specialty Drugs and High-Cost Medications
Not all plans have five tiers, but many do-especially employer-sponsored plans. Tier 4 and 5 are for specialty drugs: high-cost medications used for complex conditions like cancer, multiple sclerosis, or rare genetic disorders. These aren’t your regular prescriptions. They often require special handling, injections, or monitoring. They’re also incredibly expensive. A single dose of a Tier 5 drug can cost over $1,000. Cost-sharing here is usually coinsurance, not a copay. That means you pay 25% to 50% of the drug’s total price. If your monthly drug costs $5,000, you could be paying $1,250 to $2,500 out of pocket. That’s why many patients delay or skip these meds-41% of people surveyed by the Patient Advocate Foundation admitted to doing so because of cost.Non-Formulary: Not Covered at All
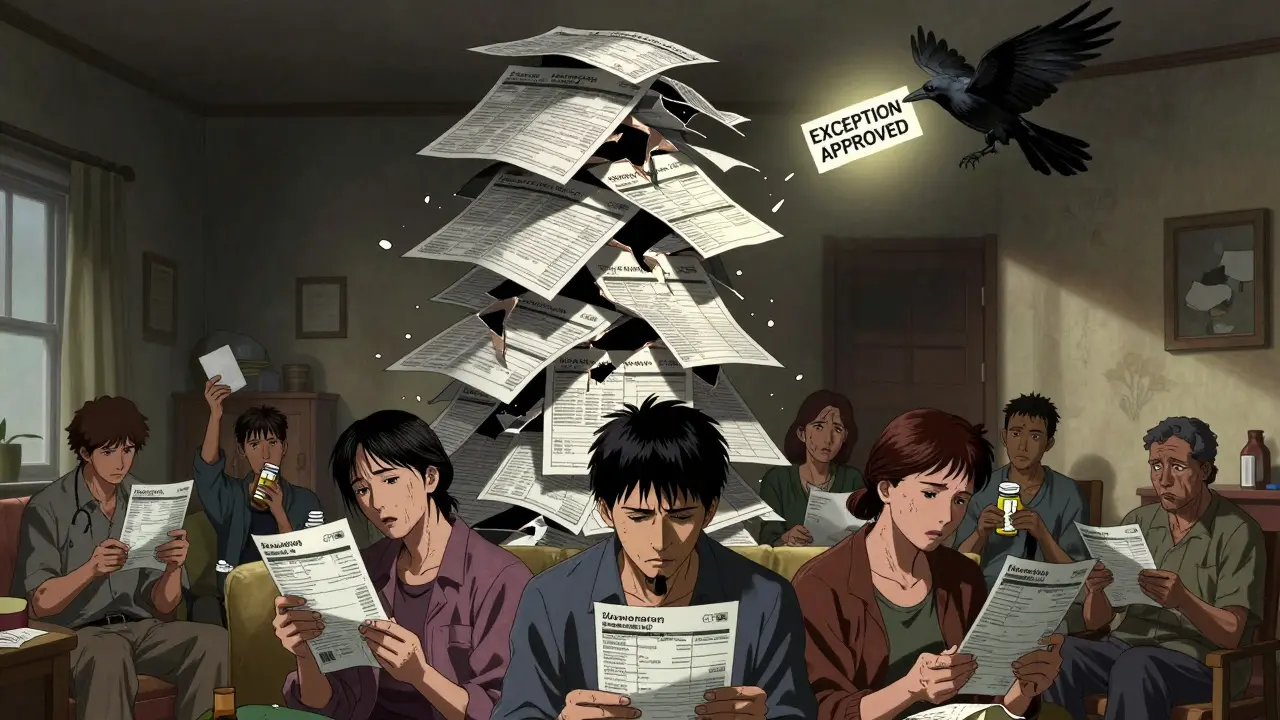
Some drugs aren’t on your formulary at all. These are non-formulary drugs. That doesn’t mean they’re unsafe. It just means your plan doesn’t cover them-unless you get an exception. Why would a drug be excluded? Maybe it’s too new. Maybe there’s no evidence it’s better than cheaper alternatives. Or maybe the manufacturer didn’t negotiate a deal with your PBM. If your doctor prescribes a non-formulary drug, you have two choices: pay full price (which can be $500+ per month), or file a formulary exception request. That’s a formal appeal where your doctor explains why you need this specific drug-usually because other options didn’t work or caused side effects. The process takes about a week. Success rates vary, but 60% of exceptions for medically necessary drugs get approved, according to the Medicare Rights Center.Why Do Tiers Change Without Warning?
You might have used a drug for years at a low cost, then one day, your copay jumps from $15 to $75. What happened? Formularies are updated every quarter. PBMs renegotiate deals with drugmakers constantly. If a new generic hits the market, your plan might move your brand-name drug from Tier 2 to Tier 3. If a drugmaker raises its price, your plan might drop it entirely. Worst part? You often don’t get notified. The plan sends a letter in the mail, but most people don’t read it. That’s why checking your formulary before each refill is critical. Most insurers have online tools-Humana’s Drug Cost Finder, Medicare’s Plan Finder, or your plan’s member portal-to look up drug tiers before you fill a prescription.How to Save Money on Tiered Formularies
You’re not powerless. Here’s what works:- Ask your doctor for alternatives. “Is there a Tier 1 or Tier 2 drug that works for this?” is a simple, powerful question.
- Use mail-order pharmacies. Many plans offer lower copays for 90-day supplies, especially for Tier 2 and 3 drugs.
- Check patient assistance programs. Drugmakers often have coupons or free programs for high-cost meds. GoodRx and NeedyMeds are free tools to find them.
- File an exception. If a drug you need is in a high tier or non-formulary, ask your doctor to help you appeal. Medical necessity is your best argument.
- Compare plans during open enrollment. If you’re on Medicare, use the Plan Finder tool. A plan with better tier placement for your meds could save you over $1,000 a year.
What the Experts Say
Dr. Erin Trish from USC found that each extra tier increases the chance you’ll skip your meds by 5.7%. Dr. Dan Mendelson of ATI Advisory says tiered formularies cut drug spending by 18-22%-but at a cost to patients who can’t afford Tier 4 or 5 drugs. The American Pharmacists Association says only 32% of plans explain how drugs get placed in tiers. That’s not transparency. That’s guesswork. Meanwhile, PBMs say tiering drives competition. They claim the $14.7 billion in annual savings from negotiated rebates lowers overall costs. That’s true-but those savings don’t always reach you.Real Stories, Real Costs
One Reddit user, u/PharmaPatient, shared that their rheumatoid arthritis drug jumped from Tier 2 to Tier 4 overnight. Their monthly cost went from $45 to $320. They appealed. It took 10 days. They got approved for a lower tier after their doctor proved no other drug worked. Another Medicare beneficiary in Texas had insulin in Tier 3-$80 a month. Thanks to the Inflation Reduction Act of 2022, insulin is now capped at $35 for Medicare patients, no matter the tier. That change alone saved millions.What’s Changing in 2025?
By 2025, more plans will use “value-based tiering.” Instead of just pricing, they’ll look at outcomes. Does this drug actually keep people out of the hospital? Does it reduce long-term costs? If yes, it might move to a lower tier-even if it’s expensive upfront. CVS Caremark already launched diabetes-specific formularies that group drugs by effectiveness, not brand vs. generic. Other PBMs are following. The trend? Simpler tiers. The average plan had 4.2 tiers in 2023. By 2027, experts predict it’ll drop to 3.5. Why? Because complexity confuses people-and confused people skip meds.Final Tip: Know Your Plan, Know Your Drugs
Don’t wait until you’re at the pharmacy counter to find out your drug costs. Check your formulary before your doctor writes the script. Use free tools. Ask questions. File exceptions. You’re not just a policy number-you’re a person who needs medicine to live. The system isn’t perfect. But understanding how it works gives you power. Use it.What is the difference between Tier 1 and Tier 2 drugs?
Tier 1 drugs are usually low-cost generics with the lowest copay-often $0 to $15. Tier 2 drugs are brand-name medications your plan prefers because they’ve negotiated a discount. Copays are higher, typically $20 to $40. The key difference is cost: Tier 1 is the cheapest option, Tier 2 is still affordable but more expensive than generics.
Why is my drug in Tier 3 when it’s not expensive?
Your plan may have a cheaper alternative it prefers-even if the drug itself isn’t expensive. Tier placement isn’t just about price; it’s about negotiation. If your drugmaker didn’t offer a rebate, or if a similar drug is available at a lower cost, your plan may place it in Tier 3 to steer you toward the cheaper option.
Can my insurance change my drug’s tier mid-year?
Yes. Health plans can update their formularies up to four times a year. They’re required to notify you in writing, but many people miss the notice. Always check your formulary before refilling a prescription, especially if you’ve had the same drug for a while.
What should I do if my drug is non-formulary?
You have two options: pay full price, or ask your doctor to file a formulary exception request. This is a formal appeal where your doctor explains why you need this specific drug-usually because other options didn’t work or caused side effects. About 60% of these requests are approved if medical necessity is clearly documented.
Are there tools to check drug tiers before filling a prescription?
Yes. Most insurers offer online formulary tools. Medicare beneficiaries can use the Medicare Plan Finder. Commercial plan members can check their plan’s member portal or apps like Humana’s Drug Cost Finder. Free tools like GoodRx and NeedyMeds also show estimated prices and patient assistance options.
How can I reduce my out-of-pocket costs for high-tier drugs?
Ask your doctor about lower-tier alternatives, use mail-order pharmacies for 90-day supplies, check for manufacturer coupons or patient assistance programs, and file a formulary exception if medically necessary. For Medicare beneficiaries, insulin is capped at $35/month regardless of tier thanks to the Inflation Reduction Act.








shubham rathee
20 Jan 2026 at 09:31So let me get this right the insurance companies are basically playing chess with our lives and we’re just pawns who don’t even know the rules? No wonder people skip meds. They don’t want us to understand they want us to suffer quietly and pay more. This isn’t healthcare it’s a rigged casino and the house always wins. I’ve seen people cry over $40 pills because their plan moved them from tier 2 to tier 3 and no one told them until they got to the counter. And the PBMs? They’re the ones laughing all the way to the bank while we’re choosing between insulin and groceries.