When you have diabetes, your kidneys are quietly at risk. Not from a sudden injury or infection, but from years of high blood sugar slowly damaging the tiny filters inside them. The earliest sign? Something simple: a small amount of protein called albumin leaking into your urine. This isn’t just a lab number. It’s your body’s first alarm bell for diabetic kidney disease (DKD). And here’s the truth: catching it early, and acting fast, can stop it in its tracks.
What Is Albuminuria, Really?
Albumin is a protein your body needs to keep fluid in your bloodstream. Healthy kidneys don’t let it pass into urine. But when the filters in your kidneys get damaged from high blood sugar, albumin slips through. That’s albuminuria.
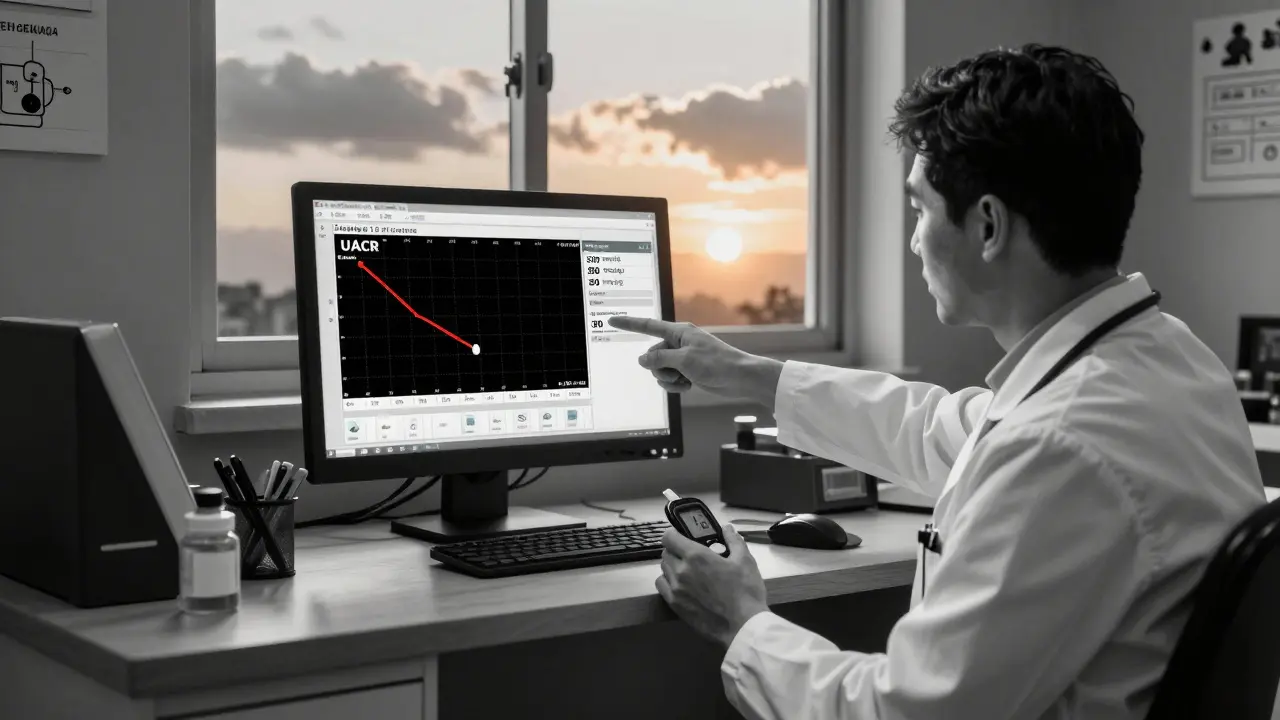
It’s not a one-time test. A single high reading doesn’t mean you have kidney damage. The numbers matter, and how you get them matters even more. The standard test is the Urine Albumin-to-Creatinine Ratio (UACR). Normal is under 30 mg/g. Anything above that? That’s a problem.
Kidney experts now use three clear stages:
- Normal: Under 30 mg/g
- Moderately increased: 30-300 mg/g (used to be called microalbuminuria)
- Severely increased: Over 300 mg/g (used to be macroalbuminuria)
Here’s what most people don’t realize: any albumin above 30 mg/g means your kidneys are already injured. There’s no such thing as "early warning" anymore - it’s damage, period. And if left unchecked, it can lead to kidney failure.
Why This Matters More Than You Think
Albuminuria isn’t just a kidney sign. It’s a full-body warning. A major study of over 128,000 people with diabetes found that those with albuminuria over 300 mg/g had a 73% higher risk of dying from any cause - and an 81% higher risk of dying from heart disease - compared to those with normal levels.
This isn’t theoretical. Every time albumin leaks into your urine, it means your blood vessels are under stress. Your heart, your brain, your legs - they’re all in danger. The kidneys are just the first to show it.
And here’s the kicker: once you pass from moderately increased to severely increased albuminuria, your chance of needing dialysis or a transplant skyrockets. But if you catch it at the 30-300 mg/g stage? You still have time.
Tight Control: The Only Proven Shield
The landmark Diabetes Control and Complications Trial (DCCT) in 1993 changed everything. It showed that people with type 1 diabetes who kept their HbA1c below 7% cut their risk of developing albuminuria by 39%. The benefits lasted decades - even after they stopped strict control. That’s called "metabolic memory." Your body remembers what you did to protect it.
For type 2 diabetes, the UKPDS study found that every 1% drop in HbA1c lowered DKD risk by 21%. That’s not a small gain. That’s life-changing.
Today, the American Diabetes Association (ADA) recommends HbA1c under 7% for most people with diabetes. But if you’re younger, healthier, and at low risk of low blood sugar, aiming for 6.5% may be worth it. Don’t chase perfection. Chase progress. Even a 0.5% drop helps.
But glycemic control alone isn’t enough. Blood pressure is the second pillar.
Pressure Matters - But Not As Much As You Think
High blood pressure crushes your kidneys. That’s why many doctors push for <120/80 mmHg. But the SPRINT trial showed that going that low in DKD patients increased the risk of sudden kidney injury. For every 47 people treated that aggressively, one ended up in the hospital with acute kidney damage.
So what’s the right target? For most people with diabetic kidney disease, 140/90 mmHg is the safe, effective goal. If you’re already on a medication like an ACE inhibitor or ARB, and your blood pressure is stable, don’t push harder just to hit a lower number. Focus on consistency.
And here’s the truth: if your UACR is over 300 mg/g, your doctor might still aim lower - but only if you’re tolerating it. No one should be pushed into risky territory for a number.
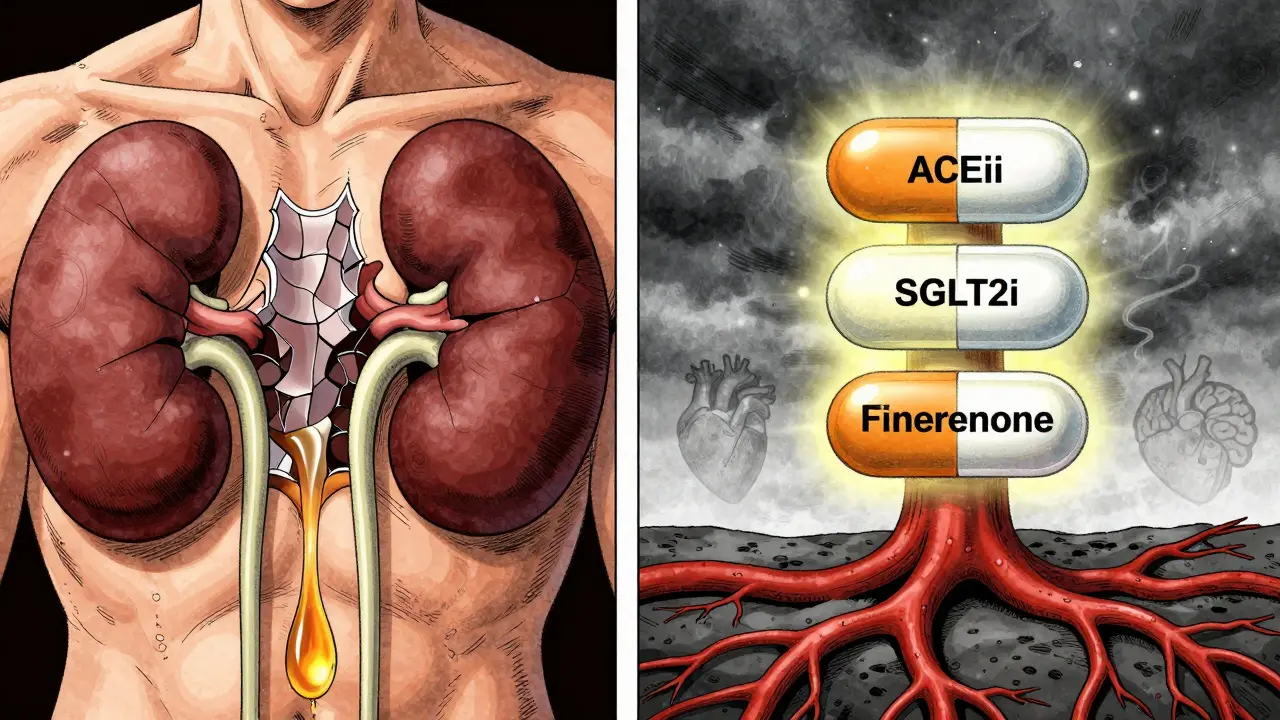
Medications That Actually Reverse Damage
Two drugs changed the game: ACE inhibitors and ARBs. These aren’t just for blood pressure. They protect your kidneys directly. The IRMA-2 trial showed that losartan - even in people with normal blood pressure - cut the progression from micro- to macroalbuminuria by 53%.
Today, guidelines say: if you have albuminuria, start an ACEi or ARB. And don’t stop at the low dose. Titrate to the maximum tolerated dose. That’s the key. Most patients get started on 25% of the full dose and stay there. That’s not enough.
Then came the SGLT2 inhibitors. Drugs like empagliflozin. The EMPA-KIDNEY trial proved they cut the risk of kidney failure by 28% in patients with UACR over 200 mg/g. These drugs work by making your kidneys flush out sugar and salt - and in doing so, they reduce pressure and inflammation inside the kidney.
Now, finerenone. A newer drug that blocks a harmful hormone system in the kidney. In trials, it cut albuminuria by 32% in just four months and slowed kidney decline by 23% over three years - even when patients were already on ACEi/ARB.
So the modern toolkit looks like this:
- ACE inhibitor or ARB - first, and at full dose
- SGLT2 inhibitor - add if not already on one
- Finerenone - add if albuminuria remains high despite the above
Yet, here’s the ugly truth: only 28.7% of people with diabetic kidney disease get all three. Why? Cost, access, lack of awareness. And that’s the biggest barrier to saving kidneys today.
Screening Is Not Optional - But It’s Often Missed
The ADA says: test UACR once a year for everyone with type 2 diabetes at diagnosis, and for type 1 diabetes after five years. It’s a Class A recommendation - the highest level of evidence. Yet, clinics report testing rates of only 58-65%.
Why? Many doctors don’t have reminders in their electronic records. Patients forget to bring samples. Some think, "If I feel fine, why test?" But DKD has no symptoms until it’s too late.
Here’s what works:
- Point-of-care urine strips - test in the clinic, get results in 10 minutes
- Pharmacist-led follow-up - they call patients who miss tests
- EHR alerts - automatic pop-ups when a diabetic patient hasn’t been tested in 13 months
One clinic in Melbourne cut missed screenings from 35% to 8% using EHR alerts and pharmacist check-ins. That’s 27 more people per month who caught their kidney damage early.
What Can You Do Right Now?
If you have diabetes, here’s your action plan:
- Ask for your last UACR result. If you don’t know it, ask for a test today.
- If it’s over 30 mg/g, don’t wait. Start the conversation about ACEi/ARB.
- Ask if you’re on an SGLT2 inhibitor. If not, ask why.
- Check your HbA1c. If it’s over 7%, make a plan to lower it - even by 0.5%.
- Keep your blood pressure under 140/90. If you’re on meds, take them daily.
- Don’t let a cold, fever, or intense workout mess up your test. Wait 2-3 days after illness before testing.
Albuminuria isn’t a life sentence. It’s a signal. And with the right steps, you can reverse the damage - or stop it before it starts.
What If My UACR Is High - But I Feel Fine?
That’s exactly why this matters. Diabetic kidney disease doesn’t cause pain, swelling, or fatigue until it’s advanced. By the time you feel it, your kidneys may have lost half their function. Waiting to act because you "feel okay" is like ignoring a smoke alarm because your house doesn’t feel hot yet.
Can I Reverse Albuminuria?
Yes - especially if caught early. Studies show that if you lower your UACR by 30% or more within the first year of treatment, your risk of kidney failure drops by over 50%. It’s not magic. It’s medicine - tight blood sugar, blood pressure control, and the right drugs.
Do I Need to Avoid Protein?
No. Cutting protein doesn’t protect your kidneys. In fact, low-protein diets can lead to muscle loss, which makes diabetes harder to manage. Eat normal, balanced amounts of protein. Focus on controlling sugar, blood pressure, and taking your meds.
Is This Only for Type 1 Diabetes?
No. Type 2 diabetes causes more than 80% of diabetic kidney disease cases. In fact, most people with DKD have type 2. Screening and treatment apply to both.
How Often Should I Get Tested?
Once a year if your UACR is normal. If it’s elevated, test every 3-6 months until it improves. After that, return to annual. If you start a new medication like an SGLT2 inhibitor or finerenone, test at 3 months to see how it’s working.
Can Lifestyle Alone Fix It?
Lifestyle is the foundation - but not the whole solution. Losing weight, walking daily, cutting sugar, and not smoking help. But if you have albuminuria, you still need medication. Think of lifestyle as the ground floor. Medication is the roof. You need both.






Stephon Devereux
10 Feb 2026 at 15:15Albuminuria isn’t just a lab result-it’s your kidneys screaming for help in a language most people ignore. I’ve seen too many patients wait until they’re swollen, tired, and on dialysis before they listen. The science is clear: catch it at 30 mg/g, not 300. That 0.5% HbA1c drop? It’s not just a number. It’s extra years. Extra walks with grandkids. Extra mornings without dialysis machines humming beside you.
Metabolic memory isn’t magic. It’s biology honoring your discipline. Start now. Not tomorrow. Not next month. Now.