It’s your body. So why do so many people feel like they don’t get to pick their own meds?
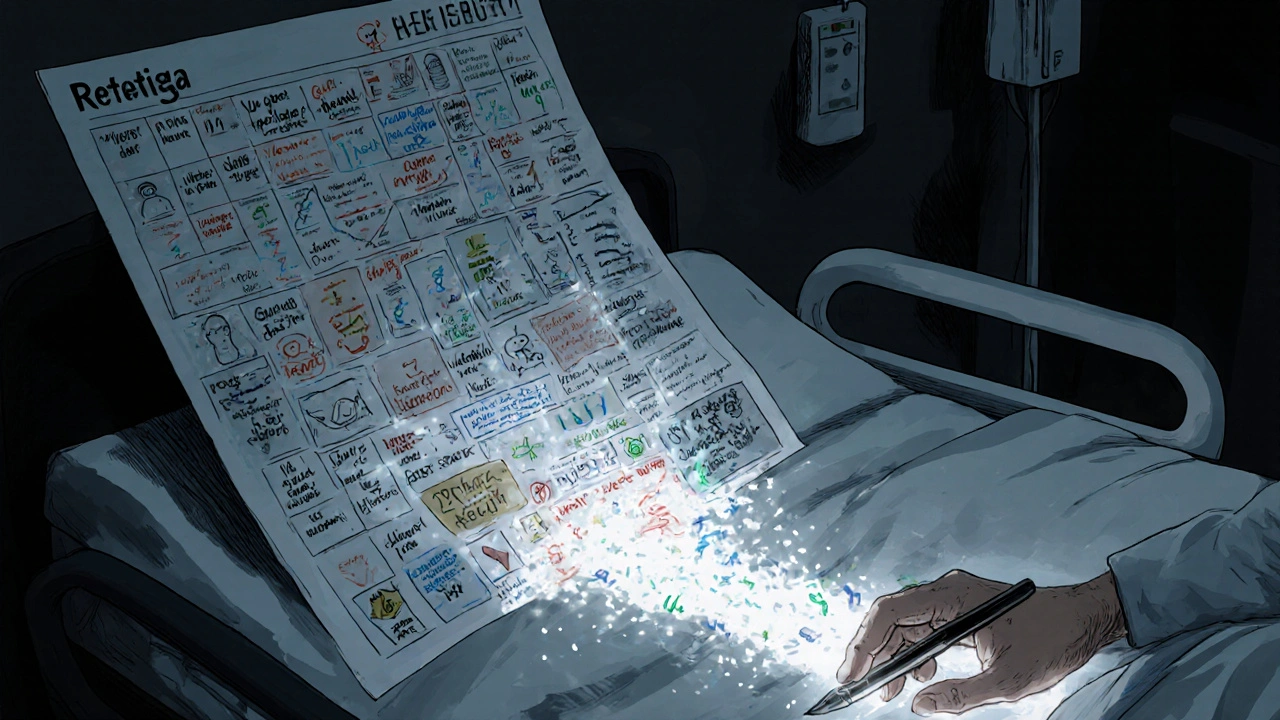
You walk into the doctor’s office with a list of symptoms. The doctor listens, runs a few tests, and hands you a prescription. No discussion. No alternatives. Just: take this.
That’s not care. That’s compliance.
Real healthcare doesn’t start with a script. It starts with a conversation. And at the heart of that conversation is something simple but powerful: medication autonomy. It’s the right - and the ability - to choose what goes into your body, even when it’s hard, even when it’s messy, even when your doctor thinks you’re making the wrong call.
This isn’t theoretical. It’s happening every day. A cancer patient refuses opioids because of her faith. A diabetic switches doctors because her provider wouldn’t talk about alternatives to Ozempic. A senior skips doses because the co-pay is too high. These aren’t just stories. They’re data points from real studies, from patient forums, from clinical trials.
And here’s the truth: when patients actually get to choose - not just nod along - they stick with their meds. Eighty-two percent continue treatment when they helped pick it. That’s 17 percentage points higher than when the doctor just decides for them.
What medication autonomy really means (and what it doesn’t)
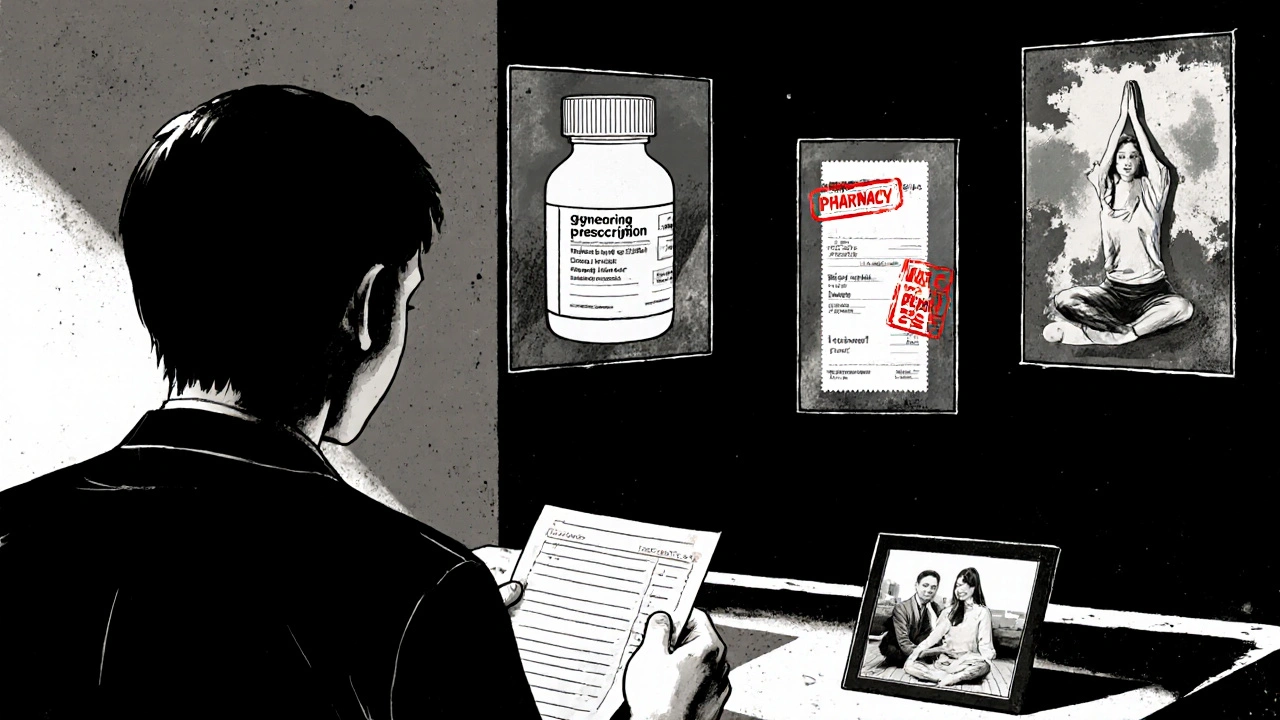
Autonomy doesn’t mean you get to demand any drug you want. It doesn’t mean you can walk in and ask for a brand-name biologic because you saw an ad. It means you get to weigh your options - with full information - and make a decision that fits your life.
That includes knowing:
- How well a drug actually works (for example, SSRIs help about half of people with depression, according to the STAR*D trial)
- What side effects you might face (like sexual dysfunction with SSRIs, which affects 25-30% of users)
- What other options exist (including cheaper generics, non-drug therapies, or digital alternatives)
- How much it costs - and what happens if you can’t afford it
And here’s the kicker: most patients don’t get this info. A 2023 survey found only 45% of primary care doctors consistently use shared decision-making for meds. Compare that to 68% for surgery - even though meds are something you take every day, for years.
Autonomy also requires capacity. You need to understand the risks, weigh the trade-offs, and communicate your choice. Tools like the MacCAT-T help doctors check this - and they’re 92% accurate. But if you’re overwhelmed, confused, or scared, you’re not making a free choice. You’re just saying yes to avoid conflict.
The hidden costs of ignoring patient choice
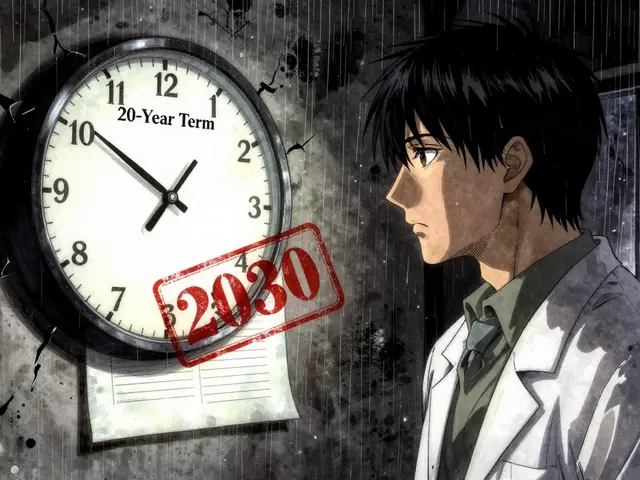
When patients don’t feel heard, they stop taking their meds. Half of people with chronic conditions quit within a year - not because they’re noncompliant, but because the treatment doesn’t fit their life.
Cost is a huge driver. In 2023, 32% of Medicare Part D users changed or skipped their meds because of price. That’s not laziness. That’s survival. And yet, many doctors still don’t ask about affordability. They assume. They prescribe. They’re shocked when the pill bottle sits untouched.
Then there’s misinformation. Social media has fueled a 40% spike in antibiotic refusal requests over two years. Patients hear horror stories online - some true, some exaggerated - and they panic. That’s not autonomy. That’s fear-driven decision-making. But the answer isn’t to shut them down. It’s to talk them through it. To say: I hear you. Here’s what the science says. Here’s what it means for you.
And let’s not forget culture. Thirty-five percent of immigrant patients say they’re uncomfortable questioning their doctor’s advice. That’s not a language barrier. It’s a power imbalance. Autonomy means flattening that hierarchy - not reinforcing it.

How real patients are taking control - and what they’re saying
On Reddit, a palliative care nurse shared this: "My patient refused opioids because of her beliefs. We built a non-opioid plan. It meant more frequent doses, but she slept better and felt respected. That’s care."
On PatientsLikeMe, a woman wrote: "My doctor pushed Ozempic and wouldn’t talk about anything else. I switched providers. I found someone who asked me what I was afraid of - and then helped me weigh options."
These aren’t outliers. They’re the rule when autonomy works.
But the data shows deep inequities. Only 49% of Black patients and 53% of Hispanic patients say they felt involved in med decisions. Compare that to 74% of white patients. That’s not a coincidence. That’s systemic.
And time? The average appointment is 15 minutes. Trying to explain drug efficacy, side effects, cost, and personal values in that window? Impossible. That’s why tools like pre-visit value clarification questionnaires are gaining traction. They give patients time to think before they walk in.
What’s changing - and what’s working
Change is happening. Slowly. But it’s happening.
Pharmacies are stepping up. Medication Therapy Management (MTM) services - where pharmacists sit down with patients to review all their meds - boost autonomy by 31%. That’s not just helpful. It’s revolutionary.
Hospitals with patient advisory councils implement autonomy protocols 2.3 times faster. Academic medical centers? 82% compliance. Community hospitals? Just 57%. The gap isn’t about skill. It’s about will.
New tools are emerging too. Shared decision-making software is a $1.2 billion market, growing fast. Platforms now track patient preferences - what they care about, what they fear, what they’ll tolerate. And the FDA is now requiring drug makers to collect patient preference data during development. That’s huge. It means future meds might be designed around real human priorities, not just clinical endpoints.
Pharmacogenomics is another game-changer. Testing your genes to see how you metabolize drugs used to cost $1,200. Now it’s $249. That means your next antidepressant or blood thinner could be chosen based on your biology - not guesswork.
How to start taking control - even if your doctor doesn’t
You don’t need a perfect system. You just need to ask the right questions.
Here’s how to begin:
- Ask: "What are my options?" Not just "What do you recommend?" But: "What else could work?"
- Ask: "What are the risks - and how likely are they?" Don’t settle for "some people get side effects." Ask for numbers. "How many out of 100?"
- Ask: "What does this cost? Is there a cheaper version?" Always. Even if you have insurance.
- Ask: "What happens if I don’t take this?" Sometimes the answer is: "Not much." And that’s okay.
- Ask: "Can we try this for a month and see how I feel?" Autonomy isn’t a one-time vote. It’s ongoing.
If your doctor brushes you off? Find someone else. Your health isn’t a transaction. It’s a partnership.
And if you’re a provider? Start here: Stop assuming. Start listening. Use decision aids. Track preferences in your EHR. Give patients time. The tools exist. The science is clear. The only thing missing is the will to change.
Why this matters more than ever
We live in a world where we choose our streaming service, our phone, our coffee order. But when it comes to what goes into our bodies? Too often, we’re handed a script and told to shut up and take it.
That’s not just outdated. It’s dangerous.
Medication autonomy isn’t about rebellion. It’s about dignity. It’s about recognizing that you know your body better than any algorithm, any guideline, any drug rep. You know what side effects you can live with. You know what trade-offs you’re willing to make. You know your values.
The future of medicine isn’t about more drugs. It’s about better conversations. About treating patients as partners - not passive recipients.
And if you’re waiting for your doctor to lead the way? You might be waiting forever. But you don’t have to wait to speak up.
Your body. Your choice. Always has been. Always will be.




Stephen Adeyanju
25 Nov 2025 at 15:37I swear to god if one more doctor hands me a script like it's a coupon for free pizza I'm gonna scream. My aunt took her meds for 3 years then just stopped because she couldn't afford them and now she's in the hospital again and nobody cares except her kids who work two jobs just to keep her alive