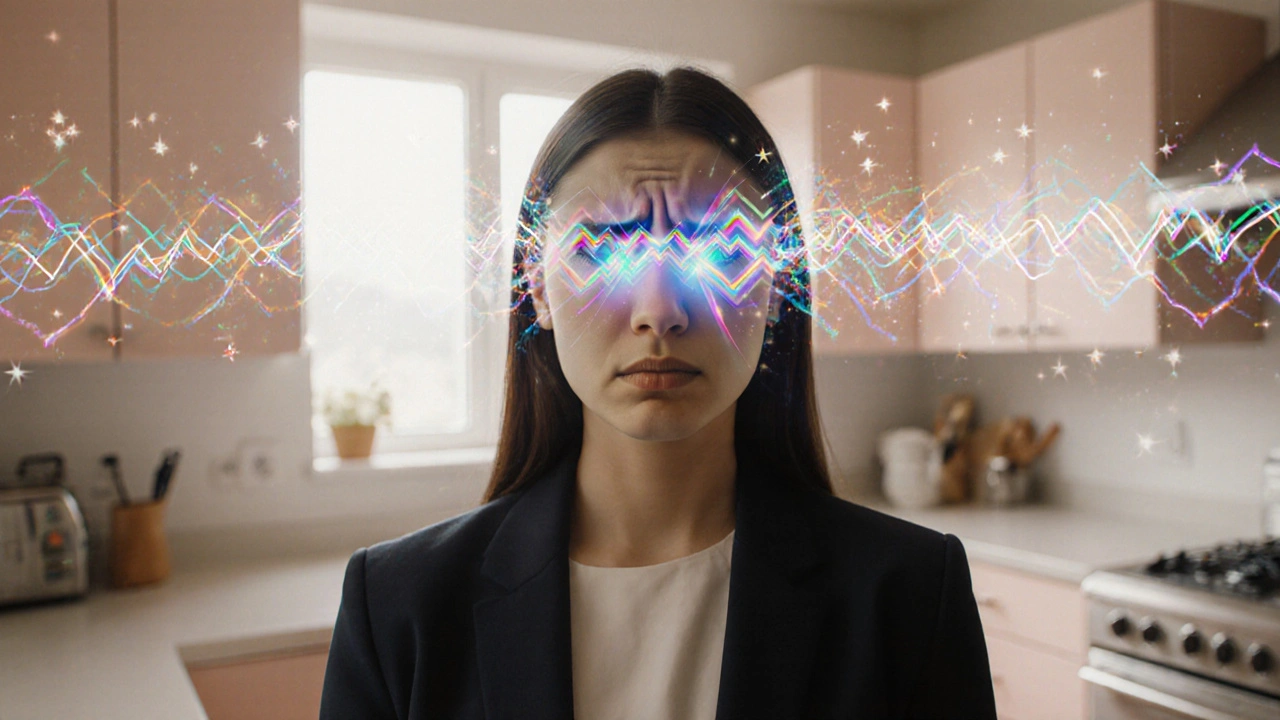
Migraine Aura is a visual disturbance that precedes or accompanies a migraine headache, typically lasting 5-60 minutes and often followed by throbbing head pain.
TL;DR
- Visual aura lasts 5‑60 minutes, showing flashes, zig‑zags or blind spots.
- It’s caused by cortical spreading depression, a wave of neuronal activity.
- Distinguish aura from retinal migraine, optic neuritis, or stroke.
- Diagnosis relies on history and, if needed, eye and brain imaging.
- Management includes acute meds, preventive drugs, and trigger control.
What Is a Migraine Aura?
When the brain’s visual cortex misfires, you may see bright spots, shimmering lines, or temporary blind patches. This episode is called a visual aura. It’s not an eye problem; it originates in the brain and usually resolves before the headache hits.
Studies from the International Headache Society show that about 25% of migraine sufferers report an aura, and up to 40% of those experience visual symptoms as the dominant aura type.
How a Visual Aura Looks
Typical patterns include:
- Scintillating scotoma: a flickering, jagged arc that expands outward, often described as a fortification pattern.
- Flashing lights or zig‑zag lines that move across the visual field.
- Temporary blind spots (negative aura) that may affect one eye.
- Distorted vision (metamorphopsia), where objects appear stretched or compressed.
These symptoms usually start in the peripheral vision and progress toward the center, lasting a few minutes before fading.
Why It Happens: Cortical Spreading Depression
The leading theory links aura to cortical spreading depression (CSD), a wave of neuronal depolarization followed by suppression of activity across the visual cortex. CSD triggers the release of inflammatory mediators that activate the trigeminovascular system, setting the stage for the headache phase.
Electrophysiological recordings in animal models show that CSD travels at roughly 3mm/min, matching the typical progression speed of visual aura across the visual field.
Distinguishing Aura From Other Eye Problems
Because visual disturbances can signal serious conditions, it’s crucial to know what sets migraine aura apart.
| Feature | Visual Aura | Retinal Migraine | Optic Neuritis |
|---|---|---|---|
| Origin | Brain’s visual cortex | Retina (eye) | Optic nerve inflammation |
| Typical Duration | 5-60min | 5-30min | Hours to days |
| Visual Pattern | Flashing, zig‑zag, scotoma | Transient monocular blindness | Blurred vision, color loss |
| Associated Headache | Usually follows aura | Often concurrent | Rarely |
| Urgent Red Flag | Sudden onset after age 50, focal weakness | Sudden, painless loss of vision | Painful eye movement, rapid vision loss |
If you notice new, sudden visual loss or pain, seek immediate medical attention - the symptoms may mimic a stroke or retinal artery occlusion.

Diagnosing Migraine Aura
Diagnosis is primarily clinical. Your doctor will ask about:
- Onset and duration of visual symptoms.
- Pattern of flashes or blind spots.
- Relationship to headache phases (prodrome, headache, post‑drome).
- Family history of migraine.
When the picture isn’t clear, an ophthalmologic examination rules out retinal disease, while a brain MRI can exclude structural lesions that might mimic aura.
Managing the Aura Phase
Because aura precedes pain, you have a narrow window to intervene.
- Acute treatments: Triptans taken as soon as aura begins may abort the headache in up to 30% of cases.
- Non‑steroidal anti‑inflammatories (NSAIDs) can reduce inflammation from CSD.
- Anti‑emetics help if nausea appears alongside aura.
For frequent aura, preventive options are worth discussing.
Preventive Strategies
Preventive therapy aims to lower the overall migraine burden, which in turn reduces aura frequency.
| Medication | Mechanism | Typical Dose |
|---|---|---|
| Topiramate | Modulates neuronal excitability | 25-100mg daily |
| Propranolol | Beta‑blocker, reduces vascular response | 40-240mg daily |
| Valproate | GABAergic enhancement | 500-1500mg daily |
| Botulinum toxin A | Inhibits neurotransmitter release | 155U every 12weeks |
Newer CGRP‑targeting monoclonal antibodies have shown promise in reducing aura‑related attacks, though cost can be a barrier.
Lifestyle & Trigger Control
Identifying and avoiding personal triggers can dramatically lower aura episodes.
- Sleep hygiene: Aim for 7‑9hours, consistent bedtime.
- Dietary triggers: Excess caffeine, aged cheese, and artificial sweeteners.
- Environmental factors: Bright flickering lights, strong odors, high altitude.
- Stress management: Mindfulness, yoga, or brief aerobic walks.
Keeping a migraine diary helps you spot patterns and discuss them with your clinician.
Related Concepts and Next Steps
While exploring migraine aura, you’ll also encounter related topics such as hemiplegic migraine (a rare form with temporary weakness), post‑drome (the recovery phase), and the role of genetic predisposition in migraine families. Future articles will dive deeper into each of these areas.

Frequently Asked Questions
Can a migraine aura occur without a headache?
Yes. About 10‑15% of aura sufferers report visual symptoms without ever developing the classic migraine pain. This is called "silent migraine" and still warrants evaluation to rule out other eye or brain conditions.
How long should I wait before seeking emergency care?
If visual changes last longer than an hour, are accompanied by weakness, speech trouble, or sudden severe headache, treat it as a possible stroke and call emergency services immediately.
Do over‑the‑counter supplements help with aura?
Magnesium, riboflavin (vitaminB2), and CoenzymeQ10 have modest evidence for reducing migraine frequency, but they don’t specifically prevent aura. Talk to a doctor before starting any supplement regimen.
Is it safe to drive during a visual aura?
No. The flashing lights and blind spots can impair visual processing and reaction time. It’s best to pull over safely or wait until the aura resolves before getting behind the wheel.
Can hormonal changes trigger aura in women?
Absolutely. Fluctuations in estrogen during menstrual cycles, pregnancy, or menopause are common migraine triggers and can increase the likelihood of aura episodes.










Debra Cine
26 Sep 2025 at 21:09Welcome to the migraine aura deep‑dive! 🌟