Medication Boxed Warning Checker
Check for Boxed Warnings
Enter your medication name to see if it has an FDA boxed warning. Boxed warnings are the strongest safety alerts for prescription drugs, indicating serious or life-threatening risks.
Boxed Warning Found
has a BOXED WARNING.
Key Safety Information
Updated in 2024 per FDA requirements
Why This Matters
No Boxed Warning Found
does not currently have a boxed warning.
However, all prescription drugs have some level of risk. Check your medication guide and discuss with your healthcare provider.
Search Results
Every year, the FDA updates its list of boxed warnings - the strongest safety alerts for prescription drugs. These aren’t just footnotes. They’re bold, black-bordered notices that tell doctors: this drug can kill if used the wrong way. In 2024, 47 new or revised boxed warnings were issued, up from 42 in 2023. That’s a 12% increase in just one year. And it’s not random. These changes reflect real-world harm, not theoretical risks. If you’re taking a prescription medication, you need to understand what’s changed - and why it matters for your health.
What Exactly Is a Boxed Warning?
A boxed warning, sometimes called a black box warning, is the FDA’s highest-level safety alert. It’s placed at the top of a drug’s prescribing information, surrounded by a thick black border. This isn’t decoration. It’s a legal requirement. The FDA mandates these warnings when post-market data shows a drug can cause serious, preventable, or even fatal side effects. Think liver failure from certain painkillers, heart attacks from diabetes drugs, or sudden death from antibiotics used incorrectly.
There are over 400 medications in the U.S. with active boxed warnings. That’s about 12% of all prescription drugs. Oncology drugs make up nearly a third of them - not because they’re more dangerous, but because cancer treatments often trade high risk for life-saving benefit. A drug like vincristine carries a warning that says: “Fatal if given by any route other than IV.” One wrong injection, and a patient dies. That’s the kind of risk these warnings are built to stop.
What Changed in 2024?
The biggest shift in 2024 wasn’t the number of new warnings - it was their precision. For years, many boxed warnings were vague. You’d see phrases like “monitor for liver toxicity” or “risk of serious infections.” But vague doesn’t help a doctor decide what to do. In 2024, the FDA started requiring specific actions. Now, warnings must include exact monitoring schedules. For example, instead of saying “monitor liver function,” a new warning might say: “Check ALT and AST levels at baseline, then monthly for the first six months.”
Another major change: all new warnings must now include quantified risk data. No more “some patients may experience…” Instead, you’ll see: “1.2% of patients under 30 developed myocarditis after the second dose.” That’s not guesswork - it’s data from real patients tracked through the FDA’s Sentinel Initiative, which now analyzes 200 million electronic health records. This shift means doctors can weigh actual odds, not just fear.
Immunomodulators - drugs used for autoimmune diseases like Crohn’s, psoriasis, and rheumatoid arthritis - accounted for 23% of all 2024 updates. Why? Because long-term use is revealing new dangers. Drugs like ustekinumab and secukinumab now carry updated warnings about increased risk of tuberculosis reactivation and certain lymphomas, based on five-year follow-up data from clinical registries.
Why These Changes Matter to You
If you’re on a medication with a boxed warning, these updates aren’t bureaucratic noise. They change how you’re treated.
Take warfarin, a blood thinner with a decades-old warning about major bleeding. For years, doctors knew the risk. But in 2024, the FDA added a new requirement: “Verify INR history within the past 30 days before initiating therapy.” That means if your last INR was six months ago, your doctor can’t just refill your prescription. They must order a new test. That’s a small step - but it prevents strokes and internal bleeding.
For patients on GLP-1 agonists like semaglutide (Ozempic, Wegovy), 2024 brought the first boxed warning for acute pancreatitis. The warning now states: “Discontinue immediately if severe abdominal pain occurs. Risk is highest in patients with prior pancreatitis or gallstones.” That’s not theoretical. Data from 1.2 million users showed a 3.7x higher incidence in those with gallbladder disease. Now, doctors screen for that before prescribing.
Even common drugs like NSAIDs (ibuprofen, naproxen) saw updates. While they’ve had GI bleeding warnings for years, 2024 added: “Risk increases 40% in patients over 75 with history of peptic ulcer.” That’s specific enough to change a prescription - maybe from naproxen to acetaminophen, or adding a proton-pump inhibitor.
How Doctors and Pharmacists Are Adapting
These changes aren’t just on paper. Hospitals and pharmacies are rewriting protocols.
At Henry Mayo Newhall Hospital, pharmacists now do a triple-check for any drug with a boxed warning. For fentanyl patches, they verify opioid tolerance using a documented history - not just what the patient says. For clozapine, they confirm absolute neutrophil count (ANC) results are within safe limits before dispensing. One nurse told a colleague: “I used to just click ‘acknowledge’ in the EHR. Now I have to open the lab results and read them.”
Electronic health records (EHRs) are also being updated. Instead of one pop-up alert that says “Boxed Warning: Risk of Hepatotoxicity,” systems now show tailored messages: “Patient is 72, on 20mg daily. ALT elevated last month. Recommend holding dose and consulting hepatology.” That reduces alert fatigue - a major problem where doctors start ignoring warnings because they’re too frequent or vague.
But it’s not perfect. A Medscape survey found 44% of physicians still feel boxed warnings delay emergency care. For example, a patient with sepsis might need moxifloxacin - but the EHR blocks it because of a QT prolongation warning. Some doctors override it anyway. That’s dangerous if done without understanding why.
The Real Impact: Lives Saved - and Lives Lost
The FDA estimates these warnings prevent 12,000 serious adverse events every year. That’s real people - mothers, fathers, grandparents - who didn’t die because their doctor knew to check a lab test or avoid a drug altogether.
But there’s a flip side. A 2023 JAMA study found that 43% of boxed warnings still don’t include clear monitoring steps. That means doctors are left guessing. And when warnings are too broad, they become noise. A 2021 AMA survey showed 52% of physicians feel warnings for common drugs like NSAIDs are “background noise.”
The most effective warnings? The ones that tell you exactly what to do. The NEJM study found that warnings with specific, modifiable risk factors - like “do not use if eGFR <30” - were 3.2 times more likely to change prescribing than vague ones.
And it’s not just about safety. Drugs with new boxed warnings lose an average of 22% in sales within a year. But some, like warfarin or insulin, stay in use because there’s no alternative. The market doesn’t punish necessity - it punishes avoidable risk.
What You Should Do Now
If you take any prescription medication, ask these three questions:
- Does my drug have a boxed warning? (Check the patient information leaflet or ask your pharmacist.)
- Has the warning changed in the last year? (New monitoring? New contraindications?)
- Am I being monitored the way the warning requires? (Lab tests? Frequency? Documentation?)
Don’t assume your doctor knows. Many primary care physicians aren’t specialists in the drugs they prescribe. A 2022 AAFP survey found only 63% of primary care providers could correctly recall the boxed warning for metformin, despite its widespread use.
Bring the warning to your next appointment. Ask: “What does this mean for me? What tests do I need? What happens if I skip them?”
And if you’re on a drug with a new warning - like a GLP-1 agonist or an immunomodulator - don’t panic. These changes are meant to make treatment safer, not to scare you off. But they do mean you need to be more involved in your care.
What’s Next?
The FDA’s 2023-2027 plan aims to issue 25% more boxed warnings based on real-world data. That means more drugs - especially newer ones like immune checkpoint inhibitors and long-term diabetes meds - will get updated warnings. The goal? Less guesswork. More precision. Fewer preventable deaths.
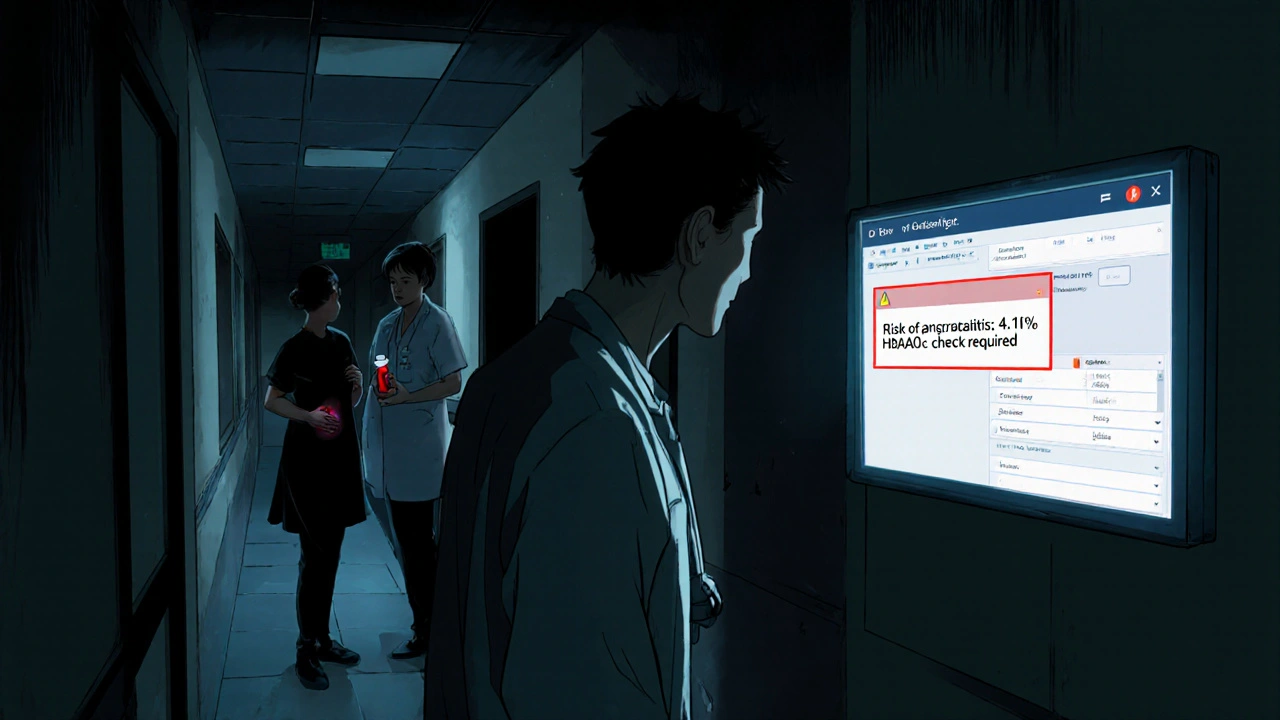
Dynamic warnings are being tested - alerts that change based on your age, kidney function, or other health factors. Imagine your EHR saying: “You’re 68, diabetic, and on this drug. Your risk of pancreatitis is 4.1%. Recommend HbA1c check every 3 months.” That’s not science fiction. It’s coming.
For now, the message is clear: Boxed warnings are evolving from blunt instruments into smart tools. They’re not meant to stop treatment. They’re meant to make it safer. And if you’re taking a prescription drug, you’re not just a patient - you’re part of the safety system.
What does a boxed warning mean for my prescription?
A boxed warning means the FDA has identified a serious, potentially life-threatening risk linked to the drug. It doesn’t mean you can’t take it - but it does mean your doctor must take extra steps to make sure it’s safe for you. This might include specific lab tests, avoiding the drug if you have certain conditions, or using it only under close supervision.
Can I still take a drug with a boxed warning?
Yes, in most cases. Boxed warnings are about risk management, not outright bans. Many life-saving drugs - like chemotherapy agents, blood thinners, or insulin - carry them. The key is whether the benefits outweigh the risks for your specific situation. Your doctor should explain why they’re still recommending it, and what safety steps they’ll follow.
How often are boxed warnings updated?
The FDA requires manufacturers to update boxed warnings within 30 days of new safety data becoming available. In recent years, updates have increased - 47 in 2024 alone. This is largely due to better post-market surveillance using real-world data from millions of patient records, not just clinical trials.
Do all doctors know about new boxed warnings?
Not always. Specialists like oncologists and psychiatrists are usually up to date, but primary care doctors may not be aware of changes to drugs they prescribe infrequently. A 2022 survey found only 63% of primary care providers could correctly recall the boxed warning for metformin. Always ask - don’t assume.
Why do some drugs get boxed warnings and others don’t?
Boxed warnings are added based on real-world evidence of serious harm - not just side effects. A drug might have many mild side effects, but if it causes one rare but fatal reaction in hundreds of thousands of users, and that risk is preventable, the FDA will issue a warning. It’s about preventable deaths, not inconvenience.
What should I do if my doctor ignores a boxed warning?
If your doctor prescribes a drug with a boxed warning without addressing the required safety steps - like skipping lab tests or ignoring contraindications - ask for clarification. If you’re still uneasy, seek a second opinion. You have the right to understand the risks. Pharmacists can also flag these issues - they’re trained to catch them.







George Clark-Roden
3 Nov 2025 at 12:49They’re not just warnings-they’re lifelines. I’ve seen a neighbor die because her doctor didn’t check her liver enzymes before restarting that one pain med. The FDA’s new specificity? It’s the difference between ‘maybe’ and ‘definitely.’ I used to think these were bureaucratic noise… until I had to sit with someone who almost didn’t make it because the system failed. Now I read every boxed warning like it’s a prayer.