Fungal Infection Treatment Selector
Find Your Best Treatment Option
This tool helps you determine the most appropriate topical treatment for your fungal skin infection based on your symptoms and medical history.
When treating fungal skin infections that also cause inflammation, Lotrisone is a topical cream that blends 0.05% betamethasone dipropionate (a potent corticosteroid) with 1% clotrimazole (an antifungal agent). It’s marketed for conditions like athlete’s foot, jock itch, and yeast infections where both fungus and redness need to be tackled at once.
Lotrisone can be a convenient one‑step solution, but it’s not the only option. In this guide we compare the combination product with the most common alternatives - both steroid‑only creams and antifungal‑only creams - so you can decide which approach matches your skin condition, safety concerns, and lifestyle.
Quick Takeaways
- Lotrisone combines a high‑potency steroid (betamethasone) with a broad‑spectrum antifungal (clotrimazole).
- For mild fungal infections without significant inflammation, a single‑active antifungal (e.g., terbinafine) is usually safer.
- When the rash is heavily inflamed, pairing a low‑potency steroid (hydrocortisone) with an antifungal can give similar relief with less risk of steroid‑related side effects.
- Prescription‑only alternatives like ketoconazole or clotrimazole‑hydrocortisone combos may be cheaper under Australian PBS subsidisation.
- Always check duration - long‑term steroid use on broken skin can thin the epidermis and increase infection risk.
How Lotrisone Works - The Science Behind the Blend
Lotrisone’s effectiveness hinges on two mechanisms working together.
- Betamethasone dipropionate is a class I corticosteroid that suppresses inflammatory mediators, reduces redness, itching, and swelling within hours.
- Clotrimazole disrupts fungal cell membranes by binding to ergosterol, halting growth of dermatophytes, candida, and some molds.
The dual action means patients often notice quick symptom relief and a faster clearance of the infection compared with using an antifungal alone.
When to Prefer a Single‑Active Antifungal
Not every rash needs a steroid. If the skin looks shiny, scaly, and there’s little redness, a pure antifungal may be the smarter choice. Here are three common single‑active options.
- Terbinafine (1% cream) - a allylamine that directly inhibits fungal squalene epoxidase, leading to rapid fungal death. Ideal for tinea pedis and tinea corporis.
- Miconazole nitrate (2% cream) - broad‑spectrum, good for candida and dermatophytes, often used for intertrigo.
- Ketoconazole (2% cream) - azole class, effective for seborrheic dermatitis and resistant fungal strains.
These products avoid the systemic risks linked to steroids, such as skin thinning, telangiectasia, or adrenal suppression, especially when used for more than two weeks.
Low‑Potency Steroid + Antifungal Combos - A Middle Ground
For patients who need some anti‑inflammatory action but want to limit steroid exposure, several low‑potency combos are available.
- Hydrocortisone 1% + Clotrimazole 1% - a pharmacy‑ready cream that offers mild steroid effect (hydrocortisone) with the same antifungal component as Lotrisone.
- Triamcinolone acetonide 0.025% + Miconazole 2% - a prescription blend used for moderate inflammation while covering a wider fungal spectrum.
These combos typically carry a lower risk of steroid‑related thinning and are suitable for longer treatment courses (up to 4 weeks) when needed.

Comparison Table - Lotrisone vs Popular Alternatives
| Product | Active ingredient(s) | Steroid strength | Antifungal class | Typical approved use | Pros | Cons |
|---|---|---|---|---|---|---|
| Lotrisone | Betamethasone dipropionate 0.05% + Clotrimazole 1% | High‑potency (class I) | Imidazole | Dermatitis with fungal infection (tinea, candida) | Fast inflammation relief + antifungal action | Risk of steroid side‑effects; prescription only |
| Hydrocortisone 1% + Clotrimazole 1% | Hydrocortisone 1% + Clotrimazole 1% | Low‑potency (class VII) | Imidazole | Mild inflammatory fungal rash | Safer steroid profile; OTC in some regions | Less powerful anti‑inflammation; may need longer course |
| Terbinafine 1% cream | Terbinafine 1% | None | Allylamine | Tinea pedis, corporis, cruris | High cure rate; short treatment (1‑2 weeks) | No anti‑inflammatory effect; may leave redness |
| Miconazole nitrate 2% cream | Miconazole nitrate 2% | None | Imidazole | Candida infections, intertrigo | Broad spectrum; inexpensive | Requires multiple daily applications |
| Ketoconazole 2% cream | Ketoconazole 2% | None | Imidazole | Seborrheic dermatitis, resistant tinea | Effective against resistant strains | Potential hepatic interaction if absorbed systemically (rare) |
Safety Profile - What to Watch Out For
Every topical medicine carries a risk‑benefit balance. Below are the main safety considerations for each group.
- Lotrisone: Prolonged use can cause skin atrophy, stretch marks, and systemic absorption of betamethasone, especially on large surface areas or broken skin. Not recommended for children under 2 years without specialist advice.
- Low‑potency steroid combos: Mainly risk skin thinning if used beyond 4 weeks. Hydrocortisone is generally safe for short courses, even on delicate areas.
- Pure antifungals: Usually well‑tolerated. Rarely cause contact dermatitis. Terbinafine may cause mild burning sensations in sensitive skin.
- Ketoconazole: Systemic absorption is minimal, but there have been isolated reports of liver enzyme elevation when applied to large areas for >2 weeks.
In Australia, the Australian Medicines Handbook advises checking for contraindications such as untreated bacterial infection or known hypersensitivity before starting any combination cream.
Cost and Accessibility in 2025
Pricing can influence the choice, especially for patients on a tight budget.
- Lotrisone remains a PBS‑listed prescription; out‑of‑pocket cost is about AU$12 for a 30 g tube, with a doctor’s script required.
- Hydrocortisone + Clotrimazole is available over the counter in most pharmacies for roughly AU$8 per 30 g tube.
- Terbinafine and Miconazole creams are generic and priced between AU$5‑AU$10.
- Ketoconazole, being prescription‑only, costs about AU$15 but may be bulk‑reimbursed for chronic cases.
If you have private health cover, many of these products are partially reimbursed, which can narrow the price gap.
How to Choose the Right Product - A Decision Flow
- Identify the primary problem: Is the rash mostly fungal (scaly, ring‑shaped) or inflammatory (red, itchy, swollen)?
- If inflammation dominates, consider a steroid‑antifungal combo. Choose Lotrisone for fast relief and when you need a potent steroid; choose a low‑potency combo if you’re concerned about side‑effects.
- If the infection is mild with little redness, start with a single‑active antifungal (terbinafine or miconazole).
- Check the treatment duration recommended on the label. Avoid any steroid‑containing product beyond 2 weeks unless supervised.
- Factor in cost and whether you need a prescription. Over‑the‑counter options are fine for uncomplicated cases.
Following this flow helps you avoid unnecessary steroid exposure while still clearing the fungus effectively.
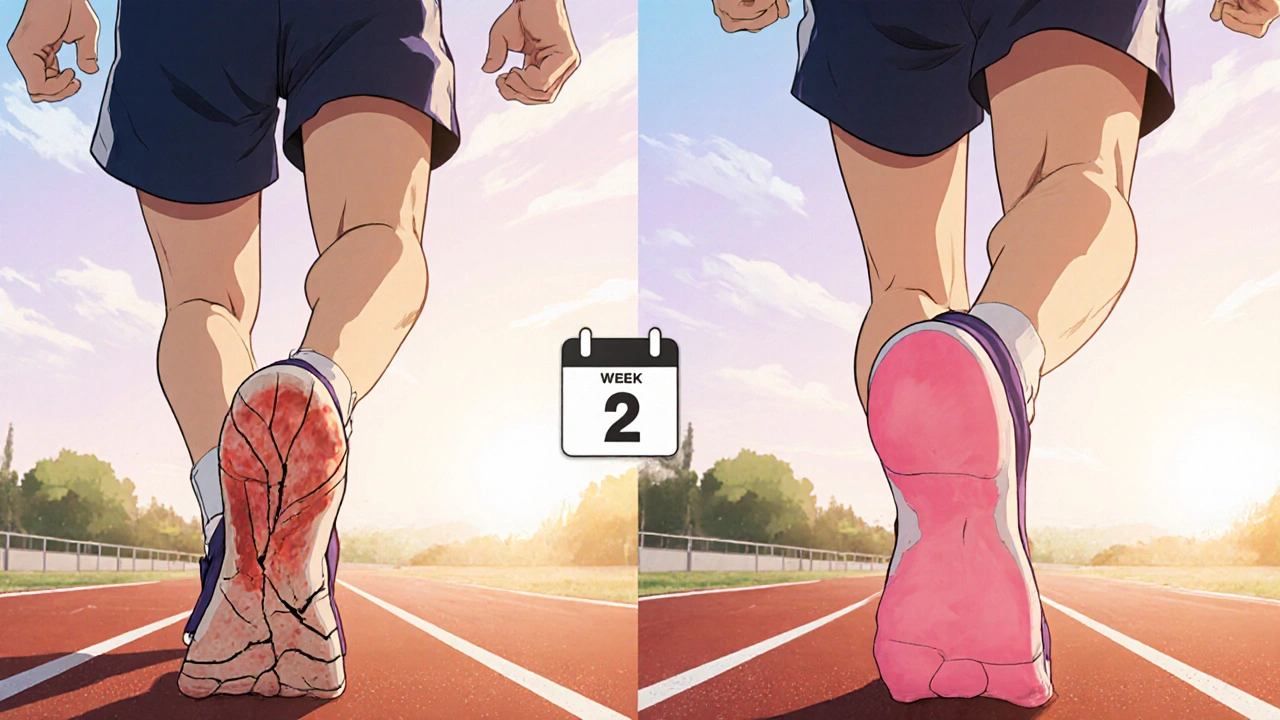
Real‑World Example: Managing Athlete’s Foot with Cracking Heels
John, a 34‑year‑old runner from Melbourne, developed tinea pedis that left his heels cracked and sore. He tried a standard clotrimazole cream, but the itching persisted because the skin around the cracks was inflamed. His dermatologist prescribed Lotrisone for two weeks, then switched to a terbinafine cream for maintenance. Within ten days, the redness subsided, and the fungal infection cleared in three weeks. John’s case shows how a short‑term steroid boost can jump‑start relief, followed by a gentle antifungal to finish the job.
Key Takeaways for Healthcare Professionals
- Prescribe Lotrisone only when both fungal infection and marked inflammation coexist.
- Educate patients about the limited duration (max 2 weeks) to prevent steroid‑induced skin changes.
- Consider lower‑potency combos for patients with a history of steroid sensitivity or for use on delicate areas like the face.
- Document any prior antifungal failures before escalating to a potent steroid‑antifungal mix.
Frequently Asked Questions
Can I use Lotrisone on my face?
Lotrisone contains a high‑potency steroid, so it should be avoided on facial skin unless a dermatologist specifically recommends it. Safer alternatives are low‑potency combos like hydrocortisone 1% + clotrimazole 1% or a plain antifungal.
How long should I apply Lotrisone?
Usually no longer than 2 weeks, and often a 7‑day course is enough for many patients. Extending beyond that increases the risk of skin thinning and systemic steroid absorption.
Is Lotrisone safe for children?
For children under 2 years it is generally contraindicated. Older children may use it under strict medical supervision, with careful monitoring for side‑effects.
What’s the main difference between Lotrisone and a hydrocortisone‑clotrimazole cream?
The steroid strength. Betamethasone dipropionate is a class I (high‑potency) steroid, while hydrocortisone is class VII (low‑potency). The antifungal component (clotrimazole) is the same.
Can I switch from Lotrisone to a pure antifungal without a wash‑out period?
Yes, once you finish the prescribed Lotrisone course, you can immediately start a pure antifungal like terbinafine for continued treatment. No wash‑out is needed because the steroid is topical and clears quickly.
Choosing the right topical treatment boils down to balancing inflammation control with antifungal potency, while keeping safety and cost in mind. Whether you opt for Lotrisone’s one‑stop solution or a tailored combo, the goal is the same: clear the infection fast and keep the skin healthy.











Casey Cloud
21 Oct 2025 at 14:02When you have a fungal infection that is also inflamed the first step is to confirm that both components are present. A visual check for scaling, redness and itching usually points to a mixed picture. Lotrisone delivers a potent steroid and an antifungal in one tube which saves a trip to the pharmacy. The betamethasone in it suppresses cytokine release and quickly reduces swelling and itch. At the same time clotrimazole attacks the fungal cell membrane and stops growth. Because the steroid is high‑potency you should limit use to no more than two weeks unless a dermatologist says otherwise. For mild cases where the skin is only scaly and not very red a single‑active antifungal such as terbinafine works just as well with fewer side effects. Hydrocortisone‑clotrimazole mixes are a good compromise when you need a little anti‑inflammatory effect but want to keep the steroid class low. Always apply a thin layer to clean, dry skin and wash your hands after each application. Avoid using the cream on large body surfaces or on broken skin for longer than prescribed because systemic absorption can occur. If you notice skin thinning, stretch marks or a rash that spreads, stop the treatment and consult a doctor. In Australia the PBS subsidises Lotrisone, making it affordable for many patients, but over‑the‑counter low‑potency combos may be even cheaper. Cost considerations are especially important for long‑term maintenance after the initial steroid boost is finished. Switching to a pure antifungal like terbinafine after a short course of Lotrisone is a common strategy that keeps the infection under control while removing the steroid. Keep a log of how many days you have used the product and set a reminder to reassess the rash after a week. Following these practical steps helps you get fast relief without compromising skin health.